Beneficial bacteria are in the news with new probiotic research now promoting their benefits. It appears the medical community has decided to “step in” and take over this core natural medicine concept and make it their own. And not surprisingly, not one article about these new studies makes mention of the fact that 90% of their conclusions about the benefits of probiotics has been known and incorporated into natural healing programs for many years. Probiotics are now being co-opted.
One of my pet peeves is how the mainstream medical community — and thus the media — trashes a particular alternative health concept for years until it finally “discovers” that same concept and claims it as their own. The examples are endless, but several certainly stand out.
- Diverticular disease
- Fiber
- Cigarette smoking as deadly
- Trans fatty acids
- High sugar intake
- Etc.
- Etc.
- Etc.
In each case, the concept, when promoted by the natural health community, was mocked and dismissed. As I’ve discussed before, diverticular disease (or bowel pockets as it was called by natural healers back in the day) was dismissed by mainstream medicine for over half a century before the medical community adopted it as their own — with no mention at all, ever, that holistic healers had nailed it long ago and had been saving people’s lives for many years by preventing and eliminating it. In fact, the standard line from the medical community during that half century of denial was, “We’ve been opening people up for years in surgeries and autopsies, and we’ve never seen any sign of this mythical disease.” But it’s hardly mythical anymore. We now know that diverticular disease will afflict virtually everyone eating a first world diet…if they live long enough. As for cigarette smoking, while the alternative healers were screaming about its dangers for decades, the medical community was promoting its virtues for weight-loss and running “physician tested and approved” ads for cigarette companies in the Journal of the American Medical Association.1 HemOnc Today. “Cigarettes were once ‘physician’ tested, approved.” Healio. March 10, 2009 (Accessed 22 June 2012.) <http://www.healio.com/hematology-oncology/news/print/hematology-oncology/%7B241D62A7-FE6E-4C5B-9FED-A33CC6E4BD7C%7D/Cigarettes-were-once-physician-tested-approved> And then there’s trans fatty acids. Even as those of us in the alternative health community were identifying artificial trans fats as one of the single biggest contributors to heart disease and premature death, the medical community was promoting their virtues and advising their patients to switch from butter to high trans fat margarine — for health reasons. Now of course, they are at the forefront of the “ban trans fatty acids” movement — and once again, without any acknowledgement of the role the alternative health community played in bringing this issue to the fore.
But other than bruised ego, why is this such a big deal?
The problem is that the medical community gets to have their cake and eat it too — and the rest of us pick up the health tab. For all the years the medical community derides a concept — detoxing would be a current example — they get to score clever media points with their mocking articles and poorly conceived studies. Unfortunately, millions of people are dissuaded from incorporating these life saving concepts into their lives. How many deaths was JAMA responsible for when they ran ads promoting cigarettes? And then, years later when they co-opted the issue by adopting it as their own, without giving even a tip of the hat to natural healers who pioneered the trail, they “take it away” from the alternative community, and deny its validity to the people who discovered it. (As the old saying goes, “You can always tell the pioneers. They’re the ones with the arrows in their backs.”) This allows mainstream medicine to continually dismiss complementary medicine as placebo based, or unscientific. After all, it didn’t work when they were mocking it. And it has nothing to do with alternative health when they take it over. It’s a rigged game.
That said; let’s take a look at the flurry of new probiotic studies that signal the first step in the co-option of beneficial bacteria.
Probiotics Are More Necessary than We Ever Thought
Within the human body, it is estimated that there are 10 times as many microbial cells as human cells, and the vast majority of them are actually beneficial and “support” our biological functions. These symbiotic microbial partners perform a number of metabolic reactions that are not encoded in (and therefore not handled by) the human genome but are nevertheless necessary for human health. Therefore, when we talk about the “human genome,” if we want to truly understand what’s happening, we should think of it as an amalgam of all our human genes and the trillions of microbes that share our bodies with us. For this reason, the National Institutes of Health Human Microbiome Project (HMP) has been performing metagenomic sequencing of microbe samples from a healthy human population to address questions such as whether there is a “core” microbiome at individual body sites and whether variation in the microbiome can be systematically studied.2 The Human Microbiome Project Consortium. “A framework for human microbiome research.” Nature 486,215–221(14 June 2012) <http://www.nature.com/nature/journal/v486/n7402/full/nature11209.html> In June, they released some of their results. (Note: microbiome refers to the totality of all the microbes that live in and on us.)
Among observations that are old hat to the alternative health community, but “new” to the medical community are “revelations” such as:
- Healthy people share their bodies with more than 10,000 species of microbes — living on our skin, in the mucous membrane of our noses and mouths, and most notably, throughout the length and breadth of our intestinal tracts. However, these trillions of microbial cells are so small that taken all together they make up only about 1 to 3 percent of our body mass.
- No one has all 10,000 species. Your specific mix depends on where you live, what you eat, and your exposure to antibiotics — either therapeutically or in your food. However, only a few are unique in function, and they are present in all healthy people. The rest vary from person to person, but are redundant in benefits so that their presence is not necessarily required. Or to put it another way, a wide variety can do the same jobs.
- All told, their collective weight is upwards of six pounds in a person of 200 lbs.
- And they play a key role in keeping you healthy…and even alive.
A “big surprise” to the researchers was that harmful bacteria are present in and on almost everyone. Why it’s a surprise, I don’t know. The Centers for Disease Control has stated for several years now that 25 to 30 percent of humans are carriers for Staphylococcus aureus (the flesh eating bacteria), which has no impact on their health but can nevertheless infect others. In healthy people, harmful bacteria such as S. aureas are kept in check (unable to proliferate wildly). As I just mentioned, the researchers seemed puzzled by this and wondered why the bad bacteria harmed some people and not others. What causes some people’s bacterial population to turn unhealthy? But this is old news to people familiar with a holistic understanding of the human body. I’ve explained for years that unhealthy bacteria (not to mention viruses and other pathogens such as Candida) are always present but kept in check both by the body’s immune system and, more importantly, by “friendly” bacteria. In other words, in healthy people, there is bacterial balance. In unhealthy people there is not. Again, this is no surprise to those in the holistic community. In fact, we even have a name for a state of microbial imbalance. It’s called dysbiosis.
“This is a whole new way of looking at human biology and human disease, and it’s awe-inspiring,” says Dr. Phillip Tarr of Washington University at St. Louis, one of the lead researchers.3 Lauran Neergaard. “10,000 germ species live in and on healthy people.” Associated Press. Jun 14. (Accessed 22 June 2012.) <http://news.yahoo.com/10-000-germ-species-live-healthy-people-170516382.html> “These bacteria are not passengers. They are metabolically active. As a community, we now have to reckon with them like we have to reckon with the ecosystem in a forest or a body of water.” And like environmental ecosystems, your microbial makeup varies widely by body part. Your skin could be like a rainforest, your intestines teeming with different species like an ocean.
In addition to all of the above, the microbiome project has discovered that all of these microbes provide a less obvious, but potentially far, far more important benefit than any we have yet discussed. In the human body, there are upwards of 30,000 genes. But the microbes in our microbiome add to that total exponentially — about 8 million genes in total. And these genes replicating in the beneficial bacterial produce substances that perform critical functions in the health and development of their human hosts. For example, genes from gut bacteria aid in the digestion of certain proteins and fats. They also produce inflammation-fighting chemicals, and immune factors such as acidolin, acidophilin, and lactocidin, not to mention a number of B vitamins.
And even more amazing, the microbial populations of the microbiome are in constant “intelligent” flux to accommodate changing circumstances. For example, according to researchers in a report that appeared just last month in PLoS One, during pregnancy, the vaginal microbiome becomes less diverse and less abundant, with one particular type of bacteria dominating.4 Aagaard K, Riehle K, Ma J, Segata N, Mistretta T-A, et al. (2012) “A Metagenomic Approach to Characterization of the Vaginal Microbiome Signature in Pregnancy.” PLoS ONE 7(6): e36466. <http://www.plosone.org/article/fetchObjectAttachment.action?uri=info%3Adoi%2F10.1371%2Fjournal.pone.0036466&representation=PDF>
“We anticipated that the vaginal microbiome would alter throughout pregnancy, but did not anticipate as significant and profound a difference between pregnant and non-pregnant women,” said Dr. Kjersti Aagaard, one of the study’s authors. Why does it change? Perhaps it’s to give the fetus as healthy a passage as possible. Previous probiotic research has found differences in which first bacteria babies absorb, depending on whether they’re born vaginally or by C-section, a possible explanation for why cesareans raise the risk for certain infections.
The bottom line is that our microbiome is far more diverse and far more important than scientists previously thought. Perhaps this will give doctors yet another reason to not prescribe antibiotics so indiscriminately. Given what we have just learned about the microbiome, antibiotics are far more damaging to your overall health than doctors previously imagined. Yes, they may kill offending bacteria, but they also kill an entire support network of trillions of life forms that coexist in and on your body, which are in fact part of it and essential to your health. Any doctor that prescribes a round of antibiotics for you and then at the very least doesn’t subsequently prescribe supplemental probiotics to jump start the rebuilding process is woefully ignorant. Without that jump start, you are begging for bacteria to rebuild asymmetrically, creating a state of dysbiosis that can result in years of compromised health. Also, for similar reasons — not to mention the fact that like antibiotics, they promote the growth of super bacteria — antibacterial soaps are not recommended. But you already knew that.
Even Beneficial Bacteria Can Be Harmful When in the Wrong Place
 A study published in the April edition of PLoS ONE has found that the bacteria in our guts regulate the immune system as well as related autoimmune diseases such as rheumatoid arthritis.5 Gomez A, Luckey D, Yeoman CJ, Marietta EV, Berg Miller ME, et al. (2012) “Loss of Sex and Age Driven Differences in the Gut Microbiome Characterize Arthritis-Susceptible *0401 Mice but Not Arthritis-Resistant *0402 Mice.” PLoS ONE 7(4): e36095. <http://www.plosone.org/article/fetchObjectAttachment.action?uri=info%3Adoi%2F10.1371%2Fjournal.pone.0036095&representation=PDF> Specifically, they found that larger-than-normal populations of specific gut bacteria (usually considered beneficial) may actually trigger the development of diseases like rheumatoid arthritis in certain situations and possibly fuel disease progression in people genetically predisposed to this condition. “A lot of people suspected that gut flora played a role in rheumatoid arthritis, but no one had been able to prove it because they couldn’t say which came first — the bacteria or the genes,” said senior author Veena Taneja, Ph.D., a Mayo Clinic immunologist. “Using genomic sequencing technologies, we have been able to show the gut microbiome may be used as a biomarker for predisposition.”
A study published in the April edition of PLoS ONE has found that the bacteria in our guts regulate the immune system as well as related autoimmune diseases such as rheumatoid arthritis.5 Gomez A, Luckey D, Yeoman CJ, Marietta EV, Berg Miller ME, et al. (2012) “Loss of Sex and Age Driven Differences in the Gut Microbiome Characterize Arthritis-Susceptible *0401 Mice but Not Arthritis-Resistant *0402 Mice.” PLoS ONE 7(4): e36095. <http://www.plosone.org/article/fetchObjectAttachment.action?uri=info%3Adoi%2F10.1371%2Fjournal.pone.0036095&representation=PDF> Specifically, they found that larger-than-normal populations of specific gut bacteria (usually considered beneficial) may actually trigger the development of diseases like rheumatoid arthritis in certain situations and possibly fuel disease progression in people genetically predisposed to this condition. “A lot of people suspected that gut flora played a role in rheumatoid arthritis, but no one had been able to prove it because they couldn’t say which came first — the bacteria or the genes,” said senior author Veena Taneja, Ph.D., a Mayo Clinic immunologist. “Using genomic sequencing technologies, we have been able to show the gut microbiome may be used as a biomarker for predisposition.”
Other diseases with suspected gut bacterial ties include type I diabetes and multiple sclerosis.
“The gut is the largest immune organ in the body,” said co-author Bryan White, Ph.D., director of the University of Illinois’ Microbiome Program in the Division of Biomedical Sciences and a member of the Institute for Genomic Biology. “Because it’s presented with multiple insults daily through the introduction of new bacteria, food sources, and foreign antigens, the gut is continually teasing out what’s good and bad.” The gut has several ways to do this, including the mucosal barrier that prevents organisms — even commensal or “good” bacteria — from crossing the lumen of the gut into the human body. However, when “good” bacteria breach this barrier, they can trigger autoimmune responses. Dr. White goes on to say that the body recognizes them as out of place, and in some way this triggers the body to attack itself.
“The next step for us is to show if bugs in the gut can be manipulated to change the course of disease,” Dr. Taneja says.
As a side note (my observation, not the researchers), this study points a very interesting accusatory finger at aspirin in terms of rheumatoid arthritis. Yes, as a Cox-2 inhibitor, aspirin can be effective in reducing the pain and inflammation associated with rheumatoid arthritis; but as a Cox-1 inhibitor, it simultaneously compromises the mucosal lining of the intestinal tract (the reason it causes intestinal bleeding), and thus may facilitate the passage of the “beneficial” bacterial through the gut and into the body — thus triggering an autoimmune response and the resultant rheumatoid arthritis. An interesting epidemiological study awaits some researcher there, I should think.
Dairy Fats Contribute to Bacterial Changes that Lead to Inflammatory Bowel Diseases
Meanwhile, new probiotic research published on June 13th in the journal Nature has linked dairy fats and bacteria in the gut with the onset of inflammatory diseases.6 Suzanne Devkota, Yunwei Wang, Mark W. Musch, Vanessa Leone, Hannah Fehlner-Peach, et al. “Dietary-fat-induced taurocholic acid promotes pathobiont expansion and colitis in Il10-/- mice.” Nature 13 June 2012. <http://www.nature.com/nature/journal/vaop/ncurrent/full/nature11225.html> The researchers found that diets high in certain dairy fats changed the way food was digested and encouraged the growth of harmful bacteria. They used genetically modified mice which were more likely to develop inflammatory bowel diseases. One in three developed colitis when fed either low-fat diets or meals high in polyunsaturated fats. This doubled to nearly two in three in those fed a diet high in saturated milk fats, which are used in many processed foods.
These saturated milk fats are hard for the body to digest, and it responds by pumping more bile into the gut. This changes the gut environment and leads to a change in the bacteria growing there, the researchers said. One bacterium in particular, Bilophila wadsworthia, was identified. It thrives in the extra bile produced to break down the fats. It went from being incredibly rare to nearly 6% of all bacteria in the gut in the high-dairy-fat diet.
Commenting on this probiotic research, Dr Roy Sleator, from the Cork Institute of Technology, said: “Not only do the authors provide, what is in my opinion, the first credible explanation as to how
Western diet contributes to the unusually high incidence in inflammatory bowel disease; they also suggest an effective means of dealing with such diseases, by simply reshaping the microbial balance of the gut.” (Not consuming dairy fats in processed foods is another way to go, of course.)
We already know that a number of the proteins in dairy are highly allergenic. And now we learn that even the fats are problematic. I know there are some in the alternative health community who are strongly pro dairy. I am not. However, as I’ve repeatedly said, if you are going to consume dairy, you want it raw, organic, and grass fed.
Mutant Acidophilus May Reverse Colon Cancer
And once again in a study released last month — in this case in the Proceedings of the National Academy of Sciences — a team of researchers from the University of Florida published their findings concerning the development of a genetically-modified form of the acidophilus that greatly reduced abnormal gut inflammation and reversed colon cancer in mice. This special variant of the acidophilus bacteria halted abnormal inflammation, reduced precancerous growths, and reversed the progression of severe cancerous lesions in the large intestines of mice.7 Khashayarsha Khazaie, Mojgan Zadeha, Mohammad W. Khan,Mansour Mohamadzadeha,et al. “Abating colon cancer polyposis by Lactobacillus acidophilus deficient in lipoteichoic acid.” PNAS June 11, 2012. <http://www.pnas.org/content/early/2012/06/05/1207230109.full.pdf+html>
 In earlier studies, the probiotic research team had demonstrated that a genetically modified form of acidophilus can bring overactive immune responses back to normal. They have now found that proteins on the surface of the specially modified bacteria can act on the immune system to either cause inflammation in the gut or tune it down. In other words, it works as an immunomodulator. In their current study, the researchers removed an inflammation-causing gene from the bacterium, and the result was a new form of the beneficial bacteria that was even better at controlling disease-causing inflammation. Moreover, mice with severe cases of polyps and cancerous intestinal lesions that were fed the modified bacteria had a significantly reduced number of colon polyps compared with untreated mice, and showed no signs of active colon cancer or disease-causing inflammation.
In earlier studies, the probiotic research team had demonstrated that a genetically modified form of acidophilus can bring overactive immune responses back to normal. They have now found that proteins on the surface of the specially modified bacteria can act on the immune system to either cause inflammation in the gut or tune it down. In other words, it works as an immunomodulator. In their current study, the researchers removed an inflammation-causing gene from the bacterium, and the result was a new form of the beneficial bacteria that was even better at controlling disease-causing inflammation. Moreover, mice with severe cases of polyps and cancerous intestinal lesions that were fed the modified bacteria had a significantly reduced number of colon polyps compared with untreated mice, and showed no signs of active colon cancer or disease-causing inflammation.
According to principal investigator Mansour Mohamadzadeh, “We have demonstrated that our bacterial treatment can take on established colon cancer. “This is huge, because people don’t come to you 10 years before they have colon cancer saying, ‘I may get colon cancer; can you treat me?’ They come to you and say, ‘I have colon cancer.'”
The modified bacteria are easy and cost-effective to produce. As a treatment for humans, it is likely to be in the form of a pill like most probiotic supplements used today. Patients could receive the beneficial bacterial treatment in combination with surgery or other therapies.
For years, researchers have understood that uncontrolled inflammation in the large intestine can result in various diseases, including colon cancer and inflammatory bowel diseases such as ulcerative colitis. This new study focused on understanding how to curb immune system processes in the gut that lead to harmful inflammation. Resulting treatments could work not just for diseases of the digestive tract but also for other conditions such as diabetes and Sjögrens syndrome in which inflammation plays a major role. It also suggests that some of the hundreds of strains of probiotics currently found in the human gut (and available in supplemental form) might produce many of the same results already — if they were present in sufficient quantities. For example, probiotic research in The American Journal of Clinical Nutrition has for some time indicated that probiotics can relieve intestinal inflammation and that probiotic bacteria have anti-inflammatory qualities.8 Erika Isolauri, Yelda Sütas, Pasi Kankaanpää, et al. “Probiotics: Effects on Immunity.” Am J Clin Nutr February 2001 vol. 73 no. 2 444s-450s. <http://www.ajcn.org/content/73/2/444s.full.pdf+html> Why wait for a magic pill? Strains known to be helpful in this regard include:
- Bifidobacteria
- L. acidophilus
- L. salivarius9 Peran L, Camuesco D, Comalada M, Nieto A, et al. “Preventative effects of a probiotic, Lactobacillus salivarius ssp. salivarius, in the TNBS model of rat colitis.” World J Gastroenterol 2005 September;11(33):5185-5192. <http://www.wjgnet.com/1007-9327/11/5185.pdf>
- L. rhamnosus10 Lin PW, Myers LE, Ray L, Song SC, et al. “Lactobacillus rhamnosus blocks inflammatory signaling in vivo via reactive oxygen species generation.” Free Radic Biol Med. 2009 Oct 15;47(8):1205-11. Epub 2009 Aug 3. <http://www.ncbi.nlm.nih.gov/pubmed/19660542>
- L. plantarum11 Puertollano E, Puertollano MA, Cruz-Chamorro L, et al. “Orally administered Lactobacillus plantarum reduces pro-inflammatory interleukin secretion in sera from Listeria monocytogenes infected mice.” Br J Nutr. 2008 Apr;99(4):819-25. Epub 2007 Sep 26. <http://www.ncbi.nlm.nih.gov/pubmed/17894920>
- S. thermophilus12 Tasuku Ogita, Megumi Nakashima, Hidetoshi Morita, et al. “Streptococcus thermophilus ST28 Ameliorates Colitis in Mice Partially by Suppression of Inflammatory Th17 Cells.” Journal of Biomedicine and Biotechnology Volume 2011 (2011), Article ID 378417, 9 pagesdoi:10.1155/2011/378417. <http://downloads.hindawi.com/journals/jbb/2011/378417.pdf>
Conclusion
The microbes in our microbiome are not just helpful; they are essential. They allow us to digest food, to assimilate the nutrients in that food, and they play a huge role — just beginning to be understood — in our immune functioning and in many other processes in our bodies. And they protect our mucosal linings and skin from deadly pathogens such as flesh eating bacteria. Quite simply, we cannot live without a healthy microbiome. And yet, we are constantly attacking and destroying it.
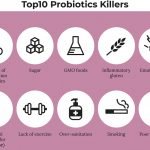
- We bathe in and drink chlorinated water. Chlorine is antibacterial; it kills all of the bacteria — good and bad — in your microbiome.
- We use antibacterial soaps, which kill all of the beneficial bacteria on your skin along with the bad, thus leaving you defenseless against flesh eating bacteria.
- We eat meat and dairy products laced with antibiotics, which destroy our intestinal flora.
- Our doctors prescribe antibiotics for us like candy, which creates a state of dysbiosis in our intestinal tracts and breeds super bacteria that can attack us later.
- And we no longer eat fermented foods to replenish the damaged populations.
Why would we expect good health when we work so hard to destroy it? Over the next few years, armed with its new understanding, doctors and the media are now likely to begin rethinking this assault on health and start working with nature rather than against it. Unfortunately, they are also likely to shove the alternative health community aside on this issue and displace natural probiotic supplements with custom engineered, prescription based versions.
Here’s hoping that, just maybe, the medical community might show a little class this time and offer an acknowledgement to all those in the alternative health community who pointed the way…but I wouldn’t hold my breath.

References
| ↑1 | HemOnc Today. “Cigarettes were once ‘physician’ tested, approved.” Healio. March 10, 2009 (Accessed 22 June 2012.) <http://www.healio.com/hematology-oncology/news/print/hematology-oncology/%7B241D62A7-FE6E-4C5B-9FED-A33CC6E4BD7C%7D/Cigarettes-were-once-physician-tested-approved> |
|---|---|
| ↑2 | The Human Microbiome Project Consortium. “A framework for human microbiome research.” Nature 486,215–221(14 June 2012) <http://www.nature.com/nature/journal/v486/n7402/full/nature11209.html> |
| ↑3 | Lauran Neergaard. “10,000 germ species live in and on healthy people.” Associated Press. Jun 14. (Accessed 22 June 2012.) <http://news.yahoo.com/10-000-germ-species-live-healthy-people-170516382.html> |
| ↑4 | Aagaard K, Riehle K, Ma J, Segata N, Mistretta T-A, et al. (2012) “A Metagenomic Approach to Characterization of the Vaginal Microbiome Signature in Pregnancy.” PLoS ONE 7(6): e36466. <http://www.plosone.org/article/fetchObjectAttachment.action?uri=info%3Adoi%2F10.1371%2Fjournal.pone.0036466&representation=PDF> |
| ↑5 | Gomez A, Luckey D, Yeoman CJ, Marietta EV, Berg Miller ME, et al. (2012) “Loss of Sex and Age Driven Differences in the Gut Microbiome Characterize Arthritis-Susceptible *0401 Mice but Not Arthritis-Resistant *0402 Mice.” PLoS ONE 7(4): e36095. <http://www.plosone.org/article/fetchObjectAttachment.action?uri=info%3Adoi%2F10.1371%2Fjournal.pone.0036095&representation=PDF> |
| ↑6 | Suzanne Devkota, Yunwei Wang, Mark W. Musch, Vanessa Leone, Hannah Fehlner-Peach, et al. “Dietary-fat-induced taurocholic acid promotes pathobiont expansion and colitis in Il10-/- mice.” Nature 13 June 2012. <http://www.nature.com/nature/journal/vaop/ncurrent/full/nature11225.html> |
| ↑7 | Khashayarsha Khazaie, Mojgan Zadeha, Mohammad W. Khan,Mansour Mohamadzadeha,et al. “Abating colon cancer polyposis by Lactobacillus acidophilus deficient in lipoteichoic acid.” PNAS June 11, 2012. <http://www.pnas.org/content/early/2012/06/05/1207230109.full.pdf+html> |
| ↑8 | Erika Isolauri, Yelda Sütas, Pasi Kankaanpää, et al. “Probiotics: Effects on Immunity.” Am J Clin Nutr February 2001 vol. 73 no. 2 444s-450s. <http://www.ajcn.org/content/73/2/444s.full.pdf+html> |
| ↑9 | Peran L, Camuesco D, Comalada M, Nieto A, et al. “Preventative effects of a probiotic, Lactobacillus salivarius ssp. salivarius, in the TNBS model of rat colitis.” World J Gastroenterol 2005 September;11(33):5185-5192. <http://www.wjgnet.com/1007-9327/11/5185.pdf> |
| ↑10 | Lin PW, Myers LE, Ray L, Song SC, et al. “Lactobacillus rhamnosus blocks inflammatory signaling in vivo via reactive oxygen species generation.” Free Radic Biol Med. 2009 Oct 15;47(8):1205-11. Epub 2009 Aug 3. <http://www.ncbi.nlm.nih.gov/pubmed/19660542> |
| ↑11 | Puertollano E, Puertollano MA, Cruz-Chamorro L, et al. “Orally administered Lactobacillus plantarum reduces pro-inflammatory interleukin secretion in sera from Listeria monocytogenes infected mice.” Br J Nutr. 2008 Apr;99(4):819-25. Epub 2007 Sep 26. <http://www.ncbi.nlm.nih.gov/pubmed/17894920> |
| ↑12 | Tasuku Ogita, Megumi Nakashima, Hidetoshi Morita, et al. “Streptococcus thermophilus ST28 Ameliorates Colitis in Mice Partially by Suppression of Inflammatory Th17 Cells.” Journal of Biomedicine and Biotechnology Volume 2011 (2011), Article ID 378417, 9 pagesdoi:10.1155/2011/378417. <http://downloads.hindawi.com/journals/jbb/2011/378417.pdf> |










Hi Doc, first I want to say
Hi Doc, first I want to say thank you for everything I ever read of yours and this article as well.This being said, not since your article on the small intestine and mineral absorption have you made my head hurt so much.Info, interrelationships, and issues came at a pace that made me wish you wrote teases for the next issue.I can and will revisit to sort out what I think I read, but right now, you really made my head hurt. Don’t dumb down for me, keep it coming. Thank you.
An excellent informative
An excellent informative article which throws light on beneficial bacteria.
Thanks Jon!
With this
Thanks Jon!
With this information there certainly is plenty to follow-up on for inquiring minds!
One section that I would like to do my due diligence on is re: “Dairy Fats (&) Bacterial Changes …”. There are several things in the study mentioned here that get my attention and beg for more information. Firstly, I would like to know whether or not the “dairy fats” came from conventional dairy products or from the traditional dairy sources. I suspect that they came from commercial sources. I recommend avoiding virtually all of the commercial dairy products which typically has been pasteurized and homogenized.
Some of my blogs that explain the reasons for that are:
“Pasteurization and The ‘Milk Problem'”:
http://curezone.com/blogs/fm.asp?i=1903458
“A Real Life Story of The Two Milks”:
http://curezone.com/blogs/fm.asp?i=1661232
and many more!
“The researchers found that diets high in certain dairy fats changed the way food was digested and encouraged the growth of harmful bacteria.” That statement was made about mice, not humans! On top of that tremendous distinction there is the fact that the mice were “genetically modified” and “… were more likely to develop inflammatory bowel diseases.” The intent in using these particular animals deserves considerable weight in the findings. So far we have no distinction made between the two main sources of dairy fat, no human subjects involved and animals that are genetically modified plus more likely to develop IBS. These are all very important facts for everyone to keep in mind when they are reading the headline findings!
“… those fed a diet high in saturated milk fats, which are used in many processed foods.”
I imagine that the manufacturers of “many processed foods” are generally getting low quality dairy fats. In any case I certainly recommend avoiding “many processed foods”!
Let’s see if I can find a source for cite #5. If so I will return!
Cheers!
Chef Jem
Great article, can you
Great article, can you suggest some brands of probiotics that you think are the best?
Actually, Baseline
Actually, Baseline Nutritionals makes all of Jon Barron's formulas for him and he can guarantee the quality. They sell a probiotic formula too: http://www.baselinenutritionals.com/products/probiotics.php
Appreciated the report. It
Appreciated the report. It leaves me like …. common sense being not obsessive may be the key. Do we know any bad/good interaction between colloid silver, MSM (DMSO), sodium chlorite/chlorine dioxide and the probiotics? Thanks Paolo
Anything with antibiotic
Anything with antibiotic properties is likely to be problematic if taken in sufficient quantities. That means, for example, that colloidal silver is a concern, but MSM is not. The stronger the antibiotic action, the bigger the concern.
In my practice, I find that
In my practice, I find that FOS feeds yeast and fungal forms, while Arabinogalactan does not, giving rise to colon-friendly butyric acid. What is your clinical experiance?
Amen, Mr. Barron I feel like
Amen, Mr. Barron I feel like it’s me, a layman and cancer survivor, talking through you.
We dont have to swallow everything the medical community says hook line and sinker although this doesnt mean that we should ignore them completely. It simply means being open to alternative options and not be quick to brand such as nonsense as experience has shown that what was scoffed at before is proving to be a healthy choice after all.
I read your article with
I read your article with great interest having gut problems following very strong antibiotics from my dentist a few years ago. However, all the articles tell how much we need this bio diversity in gut bacteria but no-one tells us how to get them back! Research says that we have between 300 to 1000 different strains of bacteria in our guts. If the antibiotics kill most of them how do we get all this diversity back? The most strains I have seen in a commercial product is 14. It seems that there are only two ways to get them back: 1. Have a fecal Transplant. (Ugh!) Or 2. Drink un-pasteurised colostrum – ideally human. I would have thought that by now there would be Commercial sources of probiotics cultered from human colostrum for sale to the public, unless, of course, there is a fear of passing on disease causing bacteria from the donor. I am in the process of ordering raw cow's milk to see if this helps. Regards Les
Start with a good supplement,
Start with a good supplement, which will rebuild the key colonies and prevent bad bacteria from taking hold. Over time, as you eat a variety of fermented foods and touch your mouth with your hands, the other populations will rebuild over time.
Its incredibly sad the way
Its incredibly sad the way the mainstream medicine tries to discredit alternative health when they take and remake a health product long discovered by the alternative community. Thanks for the wonderful article.