In the last issue of the newsletter, we explored the anatomy and physiology of the liver from a natural health perspective. In this issue, we get to reap the reward for our diligence. We cover what can go wrong with the liver, how doctors test for it, and what you can do about it — again from a natural health perspective. In addition, we will spend some time on the gallbladder and biliary tree, the bile ductwork that ties everything together. Considering that gallbladder removal (cholecystectomy) is now one of the most common surgeries in the world, with over a half million performed each year in the U.S. alone, that should be of interest to a number of people. In fact, roughly 20 million Americans suffer from gallstones, and 750,000 of them undergo cholecystectomies each year. There are 800,000 hospitalizations and $2 billion spent annually on gallbladder disease in the U.S. The bottom line is that gallbladder surgery pays for many boats for many doctors every year — and there are far better, less expensive ways to deal with the problem.
What can go wrong with the liver
As we learned in the last issue of the newsletter, the liver is amazingly resilient and, at the macroscopic level, not much goes wrong with it. Because it is so well protected, it is rarely affected by trauma, but when it is (automobile accidents, war, etc.), it is often fatal because of the large blood supply that serves it. Likewise, although primary liver cell cancer is common in Africa and Asia (related to a very specific combination of “insults” to the liver’s cells), it is very rare in the United States and the rest of the developed world where those insults tend not to exist. Although hepatitis (particularly hepatitis B) and cirrhosis can be contributing factors, the primary cause of hepatocellular carcinoma is aflatoxin B1.
Liver cancer
Aflatoxin B1 is the most potent liver cancer-forming chemical known. It is a product of a mold called Aspergillus flavus, which is found in food that has been stored in a hot and humid environment (common storage conditions in much of the third world, especially Southern China and Sub-Saharan Africa). This mold is found in such foods as peanuts, rice, soybeans, corn, and wheat (all staples in the third world). It is thought to cause cancer by producing changes (mutations) in the p53 gene. These mutations work by interfering with the gene’s important tumor suppressing (inhibiting) functions. Generally, both hepatitis B and aflatoxin B1 are required for hepatocellular cancer.
That said, metastatic cancer, which is carried to the liver from other organs (think back on how the portal system feeds blood from the intestinal tract, pancreas, and spleen through the liver) is very common.
Hepatitis A
Hepatitis A is a viral disease that affects the liver. Transmission can occur through:
- Direct person-to-person contact
- Exposure to contaminated water or ice
- Contaminated shellfish (think oysters on the half shell)
- Fruits, vegetables, or other foods that are eaten uncooked and that were contaminated during harvesting or subsequent handling.
The symptoms of hepatitis A are fever, lack of appetite, nausea, and fatigue, and then jaundice. Jaundice is a yellow or orange tint to the skin or whites of the eyes. Some persons with hepatitis A will have no symptoms at all — especially children. The symptoms of hepatitis A, if you have them, usually last about one or two weeks, and, in most cases, no specific treatment is required in order to get better. Infected persons shed the virus in their stools from a week or two before symptoms begin until a few days after jaundice begins. Because of this, persons who are ill with hepatitis A should not work in restaurants, child care centers, or nursing homes until their symptoms have resolved.
The hepatitis A IgM test is used to screen for early detection of infection and is used to diagnose the disease in patients with evidence of acute hepatitis. Hepatitis A IgM is the first antibody produced by the body when it is exposed to hepatitis A. On the other hand, hepatitis A IgG antibodies develop later and remain present for many years, usually for life, and protect you against further infection by the same virus. There is no test specifically for hepatitis A IgG antibodies, although a total antibody test (which detects both IgM and IgG antibodies) detects both current and former infection with hepatitis A and will remain positive even after receiving the hepatitis A vaccine.
Hepatitis B
The hepatitis B virus results from exposure to infectious blood or body fluids containing infected blood. Possible forms of transmission include (but are not limited to) unprotected sexual contact, blood transfusions, re-use of contaminated needles & syringes (which explains why the incidence of hepatitis B among drug users is so high), and transmission from mother to child during childbirth. It should also be noted that if you are into the latest fashion trends centered around body piercing and tattooing, you have to be extremely careful with the equipment that is used on you. Make sure the equipment is totally sterile. Using non-sterile equipment can transfer the hepatitis B virus or other blood born diseases to your body.
Also, be careful when eating out. Eating uncooked, raw food or eating from outside vendors can infect you with hepatitis B. This is of particular note when visiting third world countries, but can still be a problem in any developed country.
Symptoms of hepatitis B include:
- Loss of appetite
- Fatigue
- Nausea and vomiting
- Itching all over the body
- Pain over the liver (on the right side of the abdomen, under the lower rib cage)
- Jaundice
- Urine becomes dark in color — not yellow, but dark like tea
- Stools are pale in color (grayish or clay colored)
The danger of hepatitis B is that it can become acute, and then chronic — ultimately leading to severe liver damage. Unfortunately, there is no treatment that can prevent acute HBV infection from becoming chronic once you get it. The degree of liver damage is related to the amount of active, replicating (multiplying) virus in the blood and liver. Antiviral agents, the medical treatment of choice for chronic hepatitis B, do not work in all individuals with the disease, and may not even be required as in many cases the infection may resolve itself over time.
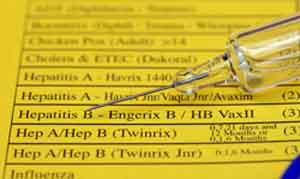
Although, it’s difficult to prevent hepatitis B from progressing if you get it, it is possible to protect yourself from getting it in the first place through immunization. The primary test for hepatitis B is for HBsAg (the hepatitis B surface antigen). Its presence indicates either acute or chronic hepatitis B infection.
Hepatitis C
Hepatitis C (HCV) is the most dangerous of the hepatitis viral infections, and it is the most common cause of chronic liver disease in North America. It is difficult for the human immune system to eliminate the virus from the body once infected, and infection with HCV usually becomes chronic. Over time (often decades), hepatitis C damages the liver and can lead to liver failure. As mentioned, it is difficult for the immune system to clear the virus — with up to 85% of newly infected people failing to clear it — and thus most people become chronically infected. It is estimated that in the U.S. alone more than three million people are chronically infected with hepatitis C, with between 8,000 to 10,000 people dying each year. In the U.S., hepatitis C is the leading cause of liver transplant surgery.
Treatment usually involves a combination of an antiviral (most often ribavirin) and alpha interferon. Alpha interferon is an antiviral protein normally made in the body in response to viral infections. The alpha interferon used in treating hepatitis C, however, is not natural. It is a recombinant form that usually involves the addition of a large molecule of polyethylene glycol to “improve” uptake, distribution, and excretion of the interferon, not to mention prolonging shelf life — and of course, increasing profits for the companies holding patents.
Peginterferon (owned by Roche), the current alpha interferon of choice, can be given once weekly and provides a constant level of interferon in the blood, whereas standard interferon must be given several times weekly and provides intermittent and fluctuating levels. In addition, peginterferon is more active than standard interferon in inhibiting HCV and yields higher sustained response rates with similar side effects. Because of its ease of administration and better efficacy, peginterferon has replaced standard interferon both when used alone and as part of a combination therapy for hepatitis C.
Combination therapy can indeed lead to rapid improvements in up to 70 percent of patients, but it often doesn’t last. Long-term improvement only occurs in 35-55 percent of patients. And unfortunately, there are side effects, which frequently include profound fatigue, headache, fever, muscle pain and chills. In fact, that’s just the tip of the iceberg.
Fortunately, there are natural alternatives. Ten years ago, I was introduced to someone who had hepatitis C and who reacted badly (extremely so) to his interferon treatments. By the time I met him, he had reached the point that he had stopped his interferon treatments, as death was preferable to the side effects associated with his treatment. As I said, those side effects can be profound. Fortunately, using a different approach, which we’ll talk more about at the end of this report, he was able to drop his numbers to undetectable levels — and maintain those for years. When I last spoke to him about two years ago, he was still symptom free after eight years — and that’s despite never giving up many bad habits including heavy, daily cigarette smoking. Since then, I have personally seen that experience duplicated several more times with other HCV patients.
Testing for hepatitis C, usually involves a series of five tests — each filling in a piece of the puzzle.
- Anti-HCV tests detect the presence of antibodies to the virus, indicating exposure to HCV. These tests cannot tell if you still have an active viral infection, only that you were exposed to the virus at some point in the past.
- HCV RIBA testing confirms the presence of antibodies to the virus. It is used to verify the results of the Anti-HCV test.
- HCV-RNA testing identifies whether your infection is active.
- Viral Load or Quantitative HCV tests determine the level of infection and are used to determine if treatment is working.
- Viral genotyping is used to determine exactly which type of hepatitis C is present. As it turns out, there are 6 major types of HCV, and they all respond differently to treatment. This test is often ordered before treatment to give your doctor an idea of the likelihood of success and how long treatment may be needed.
Cirrhosis of the liver
Cirrhosis is a degenerative disease of the liver that is often caused by alcoholism, but also may result from hepatitis and even parasites. It is characterized by formation of fibrous tissue, nodules, and scarring, which interfere with liver cell function and blood circulation and can often lead to blood backflow. Symptoms include weakness, weight loss, fatigue, abdominal swelling due to fluid accumulation, clotting defects, jaundice, and tenderness and enlargement of the liver. Tests for cirrhosis include prolonged prothrombin time and decreased albumin. Cirrhosis is untreatable and when advanced ends in portal hypertension, liver failure, hepatic coma, and death. As already mentioned, the primary tests for cirrhosis include prothrombin time (a test that measures how long it takes blood to clot) and decreased albumin. As discussed last issue, the liver makes all prothrombin and fibrinogen (clotting factors) for the blood, as well as albumin, the major blood protein. Thus, tests indicating low levels of these proteins would be indicative of liver problems.
Liver enzyme tests
A simple liver blood enzyme test is often your doctor’s first step in determining liver problems. The test is simple. Under normal circumstances, liver enzymes reside exclusively within the cells of the liver, but if the liver is injured for any reason, these enzymes spill out into the blood stream. Thus, if tests reveal them in the bloodstream, it’s an “indication” of problems. Specifically, your doctor is looking for the two aminotransferase enzymes: aspartate aminotransferase (AST or SGOT) and alanine aminotransferase (ALT or SGPT). Again, if these enzymes are found in the bloodstream, they are indicative of liver problems. They are not, however, conclusive.
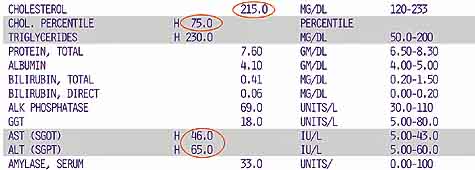
Higher-than-normal levels of these liver enzymes do not automatically mean that you have liver problems. For example, high levels of these enzymes can be caused by muscle damage — such as that produced by intense exercise. Moderate alcohol intake can also raise levels as can aspirin. Also, even if the levels are raised as a result of real liver problems, the actual levels are not indicative of the extent of liver damage. For example, patients with hepatitis A may demonstrate very high levels for one to weeks before the condition, as mentioned earlier, totally resolves itself and goes away. On the other hand, patients with chronic hepatitis C infection typically show very little elevation. Again, liver enzyme tests merely indicate a potential problem.
Bilirubin test
In addition to the liver enzyme test, the prothrombin time test, and the albumin test mentioned above, a complete liver panel will usually include one more test, the bilirubin test. Again as we discussed last issue, the liver excretes bilirubin, the broken-down pigments from dead red blood cells, by metabolizing it with bile salts and excreting it through the feces. Bilirubin is what makes our feces brown. If for some reason, bilirubin is not excreted (as in obstructive jaundice) the feces will turn clay-colored. Likewise, if bilirubin is found in the bloodstream, it’s indicative that something is amiss in the liver and that bilirubin is flowing in the wrong direction — out into the bloodstream.
Gallstones and the biliary system
As we discussed last issue, gallstones don’t start in the gallbladder; they are related to cholesterol metabolic defects originating in the liver itself. They also happen to be associated with obesity and pregnancy. Essentially, if the cholesterol produced in your liver is too thick and becomes too concentrated in the bile and sits too long in the gallbladder, it can crystallize and form gallstones. It is estimated gallstones result in some 600,000 hospitalizations and more than 500,000 operations each year in the United States alone. Bottom line: it’s one of the most prevalent digestive disorders known.
The usual treatment is laparoscopic surgery to remove the gallbladder. The surgery itself has now become so routine that it can be completed in about an hour and the patient leaves the same day — back to work the next day.
However, because it does not address the underlying cause of the problem (metabolic issues in the liver), gallbladder surgery often does not resolve the patient’s discomfort. And because it eliminates the body’s regulating mechanism for the release of bile when needed, it often creates new digestive problems of its own. In fact, after gallbladder removal, some 13% of patients report persistent pain. Another 17% report chronic diarrhea, and another 20% report intermittent digestive problems and pain. The bottom line is that although surgeons will report an almost 100% success rate for the surgery, patients will report a 50 % failure rate. It’s all a matter of perspective. The surgeon considers the surgery successful if the patient survives, there are no immediate problems, and she collects her fee without a lawsuit. The patient, unfortunately, has to live with the long term results.
The biliary tree
The biliary tree is the anatomical term for the treelike path by which bile is secreted from the liver on its way to the duodenum.
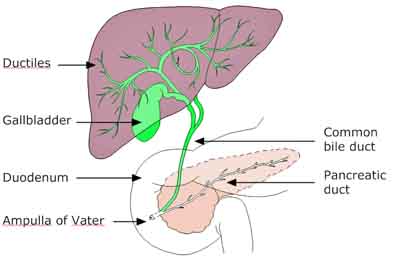
It is referred to as a tree because it begins with a multitude of small branches coming from the thousands of liver lobules which empty into the common bile duct, which is sometimes referred to as the trunk of the biliary tree. Hanging off the trunk, tucked up into the liver is the gallbladder. It is a secondary outpouching, if you will — an outpouching of the bile duct coming from the liver, which is itself an outpouching of the digestive tract. The gallbladder lies in a groove under the liver, between the two lobes, and is a soft, thin-walled sac, shaped like a fat carrot, with its narrow end pointing toward the bile ducts.
Liver duct system
Bile drains from the ultra small bile ducts (ductiles) that service each of the liver’s tens of thousands of lobules into progressively larger ducts, culminating in the common bile duct. The right and left hepatic ducts join just outside the liver to form the common hepatic duct.
Bile passing through the common bile duct exits and enters the gallbladder through the cystic duct. Most physicians refer to the gallbladder as a vestigial organ (as they do the appendix) — meaning that it’s lost most of its original function and now pretty much “gets in the way.” To them, this explains why the gallbladder does not usually empty completely, which allows gallstones to form — leading to pain, infection, inflammation, and even cancer. This also explains why they remove upwards of half a million gallbladders a year in the United States alone.
They are wrong!
The gallbladder serves a definite function. It is not vestigial. It regulates the flow of bile so that it can “push out” into the digestive tract in bursts as needed to assist in the digestion of fats. In fact, the gallbladder will contract to squeeze out stored bile when stimulated by a fatty meal. Without the gallbladder, bile merely dribbles out in a constant flow, thus being present when not required and insufficiently present when needed. This can lead to a whole series of digestive problems including poor digestion, intestinal distress, diarrhea, and an inability to fully break down fats. In fact, many people, as they age, need to take an ox bile supplement (available at all health food stores) with their meals to compensate for insufficient bile in their digestive tracts. If you have digestive problems after eating fatty meals, it’s one of the first things you (and your doctor) should look at.
It is important to understand that problems with the gallbladder rarely stem from the gallbladder itself. They stem from the liver, which if not functioning properly will manufacture bile that is prone to “stoning.” Thus removing the gallbladder does not eliminate the problem; it merely eliminates ONE place problems can manifest. Where else can problems manifest? If you follow the biliary tree down past the gallbladder, you will find that the common bile duct joins the pancreatic duct before entering the duodenum through the ampulla of Vater. And there’s the problem. Although stones and sludge formed in the liver can no longer get trapped in the gallbladder (if it’s been removed), they can still quite easily get lodged in the pancreatic duct and ampulla of Vater. This causes the digestive juices secreted by the pancreas to back up into the pancreas itself and start inflaming and digesting pancreatic tissue. This is called pancreatitis.
In other words, by merely removing the gallbladder and not addressing the underlying problem of “bad bile” being formed in the liver, you may potentially merely be moving symptoms from the gallbladder to the pancreas. Fortunately, there are alternatives. Dietary changes will often help. But the best way to optimize the health of your liver, gallbladder, and pancreas is to regularly cleanse and flush the liver and gallbladder.
The liver gallbladder flush
Of all the things I talk about in my books and newsletters, the one that medical doctors have the hardest time with is detoxes and flushes. In fact, the “scientific” community will regularly speak out against the concept. But most of that hostility comes from confusion, misunderstanding, and prejudice. Yes, it’s true that there is a great deal of “noise” that contributes to that confusion. A search on the internet shows that the word detox has been associated with everything from shampoos to footpads. On the other hand, it’s not that hard to separate the wheat from the chaff– if one wants to. Certainly there’s a whole lot of chaff in the medical community that must be ignored: hormone replacement therapy, angioplasties, and Tamiflu to name just a few.
That said, the principle of the liver/gallbladder flush is simple. You deprive the body of all fats and oils for a period of time to allow bile and cholesterol to build up in the liver and gallbladder. You then consume a drink containing a large amount of olive oil, which requires the liver and gallbladder to purge all of their bile in an attempt to digest this sudden intake of fat. This produces a figurative “wringing” action on both the liver and gallbladder causing them to empty. In addition to the purging of bile and cholesterol, a good flush will also help the liver purge accumulated fats and toxins. There are several cautions when doing a liver/gallbladder flush.
- You will want to have done an intestinal cleanse before doing the liver flush. Why? Because when the liver and gallbladder purge, they dump into the duodenum. If the intestinal tract is not flowing smoothly the purged bile and toxins can either backup into the bloodstream through the liver or be reabsorbed into the bloodstream through the intestinal tract. This can lead to a cleansing reaction.
- You will want to soften any gallstones before doing the flush. Otherwise, if the stones are large and hard, it will be quite painful (possibly even harmful) when the hard rough stones are squeezed through the bile ducts. At one time I used to recommend products such as Phosfood Liquid, Super Phos 30, and liquid extracts of chanca piedra. And they work. In the end, I designed my own softening formula that works far better and faster than these other alternatives — often in a matter of one to two hours. But more importantly this formula helps with all kinds of stones including kidney, gallbladder, and pancreatic. In any case, you will want to do one of these programs before doing a liver detox to soften the stones.
One day versus five day liver cleanses
If you search under liver flushes on the net, you will find two programs recommended — a five day program and a one day program. The principles of both programs are the same. The one day program is essentially the same as the last day of the five day program. I prefer the five day program for a number of reasons.
- You get to build the strength of the morning purge drink from one to five tablespoons of olive oil over five days. This not only provides a cumulative effect; it also allows the body to adapt, thus making the five tablespoon drink easier to handle.
- Whereas both programs will purge the gallbladder, the five day program does a much better job of purging the liver too.
- The five day program is accompanied by herbal teas and tinctures that also contain:
- Lipotropics so they help purge fats from the liver
- Antiparasitic herbs so they help flush parasites from the liver
- Liver rebuilding herbs such as milk thistle and Picrorhiza kurroa that help regenerate liver function
- And are accompanied by juice fasts that help the entire body rebuild and repair itself
What you can expect on the liver detox
 If you are so inclined (and you should be), you should examine what you deposit in the toilet during the liver/gallbladder flush. Check for “stones” which may or may not be visible. The bile from the liver gives some stones their typical green color, but also look for black, red, and brown stones, as well as stones with blood inside them. During the course of the cleanse, some people will pass many. Be glad, because the more you pass, the healthier you become. You may also find untold numbers of tiny white cholesterol “crystals” mixed in with the waste. But do not be fooled. Oftentimes, the olive oil is converted into little “soap beads” in the intestinal tract, and many people confuse these little beads with actual stones. Also, keep in mind that if you are softening your stones before doing the flush, they will develop the consistency of toothpaste — thus they will be significantly elongated when “squeezed” out and not look very beadlike at all. And if you are taking psyllium during the program (which I recommend), most of the waste will be encased by the psyllium and not be visible at all.
If you are so inclined (and you should be), you should examine what you deposit in the toilet during the liver/gallbladder flush. Check for “stones” which may or may not be visible. The bile from the liver gives some stones their typical green color, but also look for black, red, and brown stones, as well as stones with blood inside them. During the course of the cleanse, some people will pass many. Be glad, because the more you pass, the healthier you become. You may also find untold numbers of tiny white cholesterol “crystals” mixed in with the waste. But do not be fooled. Oftentimes, the olive oil is converted into little “soap beads” in the intestinal tract, and many people confuse these little beads with actual stones. Also, keep in mind that if you are softening your stones before doing the flush, they will develop the consistency of toothpaste — thus they will be significantly elongated when “squeezed” out and not look very beadlike at all. And if you are taking psyllium during the program (which I recommend), most of the waste will be encased by the psyllium and not be visible at all.
If you don’t notice anything, though, it doesn’t mean the flush is not working. Also, many people don’t have gallstones. But they do have toxins and accumulated fat in the liver, and those are being purged. In the end, though, it’s not what you see, it’s how you feel. Wait for a few days after the cleanse and then evaluate. Did you lose weight? Do you feel lighter and cleaner? Did your senses come alive? Does food taste better? Are colors brighter? Is your breathing a little easier, less congested? These are the true evaluations of the liver detox.
Go to the liver detox site
I am not going to go into the details of how to do a liver flush in this newsletter. It’s too involved to cover in a single newsletter, and we’ve covered it in great detail at the Baseline of Health® Foundation website. Everything you need to know is there including things like:
- Everything you need to buy
- Exactly how to make the morning flush drinks
- What to eat and juice during the flush
- Daily walkthroughs and hour by hour schedules
- What to do if you’re diabetic
- What to expect
- Live Q and A sessions
Check it out at: Baseline of Health Foundation Liver Detox and Blood Cleanse
And that concludes our section on the pancreas, liver, and gallbladder. When next we return to our exploration of the anatomy and physiology of the intestinal tract from a natural health perspective, we will pick things up with the small intestine.












Hi. I'm having some digestive
Hi. I’m having some digestive pain. I’ve had an xray & an ultrasound in the last week. My doctor has not contacted me with the results yet. Would you suggest doing the cleanse with the pain I’m experiencing? If I eat items from the no no list I awake with pain in my upper back, hurting to breathe & move. It’s gas, it works its way out but very painful, until dissapated. I am taking a product by Standard Process AF Beta Food, 3 3times a day. This has helped tremendously! I’ve read your article & would rather not have my gallbladder out. Please advise. Thanks so much!
Sincerely,
Carol J Vandermeer
I have my gallblader removed
I have my gallblader removed because of a lot of big stones, now my liver is not fuctioning well and I`m a diabetic what can i do to help my liver to finction well?
Hi Barry,
Hi Barry,
We can not diagnose or treat, merely provide information. I would read Jon Barron’s book if you want to start looking at supporting your health with natural remedies.
Can a person with Hepatitis C
Can a person with Hepatitis C (genotype 1a) do a liver cleanse?
For obvious legal reasons, we
For obvious legal reasons, we cannot diagnose or prescribe for specific medical issues—merely provide information. That said, you might find the following testimonial informative. http://www.jonbarron.org/detox/liver-cleanse-Hepatitis-C
I have my son who is 20 that
I have my son who is 20 that has mono for 4 weeks now he is better with the energy but the liver enzyme still allevated
Any suggestions please thank youb
One of the many functions of
One of the many functions of the liver is to make factors to help the human immune system fight infection. This will be reflected in elevated ASL and AST liver enzymes. The best thing you can do is support your body’s immune system and supplement with natural antivirals.
Hello, Im a 37yr. old male
Hello, Im a 37yr. old male who drinks probably 6-12 beer’s a day for over 10yrs.I have had a few blood tests that show very high liver enzymes over the past 6 months. My doc told me to quit drinking cold turkey but I don’t want to I enjoy it.I also asked him about liver detox or any of those types of thing’s and he said it doesn’t work. I was wondering if there is any hope for me and im scared now, I have 2 kids that I wanna watch grow up. I have a liver ultrasound scheduled for next weak please let me know your opinion of what I should do thx Dan
Liver detoxes do help…after
Liver detoxes do help…after you stop drinking. If you can’t stop, you should check out several rehab facilities to support you. Once you quit, then you can begin to repair the liver naturally. You can do more damage to try and detox while still drinking, but you probably knew that.
After doing the flush this
After doing the flush this last Thursday, I passed at least 400 pieces. I took 20 of them to my doctor on Friday for him to see. He told me that they were unformed bm from inside of my intestines, and that I do not have liver or gallbladder issues. He had done a blood screen for me last year, and he told me that my levels were good. Despite that, my eyes are yellow and red, having a growth on my left eye. My doctor told me that he doesn’t know why my eyes are yellow, but there is no cause for concern. He said the growth is Surfer’s Eye (exposure to UV light) and he can remove that when it gets large enough. I had blood tests two months ago, and my vitamin levels were low (despite the fact that I eat relatively healthy and take vitamins every day.) He gave me a B12 shot at that time, and prescribed me vitamin D3 capsules to take once a week and told me to keep taking my vitamins. I also had abdominal bloating, back pain and he diagnosed me with “asthma with allergies” which he prescribed me an inhaler for. The skin under my eyes was yellow, and when I would wake up in the mornings, my palms would be swollen (and my lower legs) and my hands would be yellow. I had two liver spots on my left hand. I was diagnosed with hypothyroidism 9 years ago, and my dosage for levothyroxine has increased to 100 mcg over time. And, I was tired all of the time.
After I did the flush, my back pain went away the same day and it has not returned (and have been thinking about all of the dollars I spent at the chiropractor for years and the amounts of ibuprofen I’ve taken for the pain…). I have not had to use my inhaler since Wednesday (it’s now Sunday) although I have been coughing up a lot of congestion. The “squirrel” feeling in my chest is gone. The liver spots on my left hand are gone. My sense of smell has changed and the way that I see has changed. Everything seems more beautiful and vibrant. My eyes (themselves) are still yellow and streaked with red, but my hands are not yellow and swollen in the mornings now and my legs are not retaining water now. The bloating in my abdomen in gone. I have been sleeping a regular 8 hours instead of 10-12-14 hours. The yellow under my eyes is gone.
What should I do now? I’ve eaten three full but not excessive meals since Wednesday and have been drinking 100% apple juice without sugar and water with lemon. I don’t feel hungry much now. I don’t know how to moderate what I need now. My eyes are still yellow. I haven’t taken my vitamins since Tuesday (in preparation for the flush) nor have I taken the levothyroxine or ibuprofen. What if I quit taking those things forever? Can I live free from my pills?
For obvious legal reasons, we
For obvious legal reasons, we cannot diagnose or prescribe for specific medical conditions—merely provide information. In addition, it is also a practical impossibility to accurately diagnose complex conditions by email. There is simply too much that is not effectively communicated. That said, some comments on your question.
You doctor is most likely correct about not passing stones. As Jon Barron has pointed out on numerous occasions, “people often confuse the little “soap” beads that the body can make out of olive oil in the intestinal tract as stones.” But that doesn’t really matter, because as he also makes clear. “The fact the body produces “soap stones” doesn’t mean that it isn’t also flushing real gallstones. In the end, though, it’s not what you see that’s significant–it’s how you feel.” And as you pointed out, you felt much better after completing the cleanse. Remember, the liver cleanse, if done properly is about much more than just passing gallstones. It’s about flush fats and toxins from the liver and promoting the rebuilding of damaged liver tissue.
Also, what flush did you do? (That was a rhetorical question.) You mention doing “the flush last Thursday.” But the flush Jon Barron recommends takes five days to complete. If you didn’t do Jon’s flush, did you use the liver tincture and tea? As you will see in a moment, this becomes important in answering your main question of what you can do moving forward.
Keep in mind that there are many possible causes for yellow eyes. Although liver/gallbladder problems figure prominently in most of them, there are a number of possible causes outside of liver problems.
As to what to do moving forward:
I was wondering about
I was wondering about Hepatitis B and its treatment. The article said that it’s difficult to stop the spread of it, yet my sister who contracted it from a hospital in Nairobi (blood transfusion) was successfully treated for her hepatitis years ago.She is in good health now and doesn’t seem to have lasting effects from Hep B.
Hi Jon,
Hi Jon,
I’ve recently been thinking more about the functions of our liver and gall bladders. I found this article really helpful and informational. I have been wanting to give those organs a fresh and healthy start but hadn’t thought of the repercussions of doing it without first an intestinal cleanse and softening of the stones. In trying to research this topic, I keep getting sent to sites or cleanses for the colon. Do you have a intestinal cleanse method you could suggest or is cleansing the colon enough? I appreciate your help on this.
Thank you,
Jon Barron’s Colon Cleanse is
Jon Barron’s Colon Cleanse is one of the most cleansing, healing, and soothing you will find. In this article, Jon states what a colon cleanse should do: http://www.jonbarron.org/article/death-begins-colon#.VubjecdZsZI
“Specifically, it must serve to:
You may want this link to: http://www.baselinenutritionals.com/products/intestinal-detox-package.php
I am a US expat living in the
I am a US expat living in the Czech Republic. March 4th 2016 I had a severe gallbladder attack which led to 8 days in the hospital. Removal of the gallbladder was of course recommended but I would have to wait until the infection and inflammation was cleared up….put on antibiotics for three weeks. In the meantime I start researching how I could save my gallbladder. Problem is that my one stone is 2.8 cm. which is too big to pass using a flush program. I have now found in China a hospital and Dr. that has a “relatively” new operation for actually removing the stone and not the gallbladder. The operation cost about $5500 plus the flight to China and takes about 10 days. Is there any other way to get rid of my stone other than the surgery in China or having the complete gallbladder removed. I’m 64 but healthy all my life and very young spirited.
For obvious legal reasons, we
For obvious legal reasons, we cannot diagnose or prescribe for specific illnesses. Merely, provide information. For that reason, our site contains a great deal of information on natural methods for both softening stones and expelling them from the body. You need to read over that information and then make your own decisions.
Some helpful links:
https://jonbarron.org/kidney-detox-faqs
https://jonbarron.org/detox/barron-report-kidney-blood-cleansing-4a
https://jonbarron.org/article/kidney-detox-testimonials
Since even soft stone’s need
Since even soft stone’s need to be squeezed out like bile, how can this happen if you do not have a gallbladder to contract and squeeze? The liver does not have that function.
You don’t have stones in the
You don’t have stones in the liver. Stones form in the gallbladder when imbalanced bile hangs around too long in the gallbladder and hardens. Gallstones may form if bile contains too much cholesterol, too much bilirubin, or not enough bile salts. What is purged from the liver is accumulated fats, cholesterol, and bile—as they flow out once the channel is cleared for them to flow.
People who don’t have
People who don’t have gallbladders still get gallstones stuck in their bilary duct. Claiming that only stones can form in the gallbladder is absurd. Saying well that is just a bunch of bile, cholesterol, bile etc is like saying there is no such thing as ice because that is just really a bunch of water. This doesn’t mean some stones won’t form in gallbladder too. They form where the right conditions exist.
Yes, you are technically
Yes, you are technically correct. It is possible to have gallstones in the bile duct after your gallbladder has been removed, but the numbers are very, very small. Approximately 3-4% of people who have had their gallbladder removed will have stones in their bile duct sometime later in life. And of that 3-4%, a significant number are people who had tiny stones left in the bile duct at time of gallbladder removal that grow and become a problem. The number of people who have stones newly formed in the bile duct is very, very small—for the simple reason that if the bile has less time to hang around, it has less chance to harden into stones. But again, stones don’t form in the liver itself other than in the rarest of circumstances. They form after the liver produces bile—and if that bile has had a chance to harden in the gallbladder and to a much lesser extent in the bile duct. Note gallstones in the bile duct if you still have your gallbladder are far more common as the bile can remain trapped in the bile duct by a blocked gallbladder and have a chance to harden.
Gallstone can be made up of
Gallstone can be made up of bundles of smaller stones. Smaller stones made up of gravel and gravel resulting from sludge etc. Whether one thinks there are stones in the liver may be a definition game of what constitutes a stone so everyone may be technically correct.