We examine the anatomy of the respiratory system and learn about its two primary functions. First, it is an exchange system – swapping out carbon dioxide for oxygen. Second, it is instrumental in maintaining the acid/alkaline pH balance in your body.
Back in 2007, I wrote a four part series on the anatomy and physiology of the cardiovascular system. The idea behind the series was that by looking at the basic anatomy and physiology of the various body systems from a doctor’s perspective, we gain a unique perspective. Once we understand the underlying basis of medical treatments used to correct problems in that system, we can make informed decisions as to which of those treatments and medications actually make sense for us…and, more importantly, what natural alternatives might actually work better. So with that in mind, let’s go back to our exploration of anatomy and physiology by exploring the respiratory system.
The primary functions of the respiratory system
At its simplest level, the respiratory system, for all its complexity, really has just two primary functions. First, it is an exchange system that swaps out carbon dioxide, the byproduct of metabolism, for oxygen. In addition, it is instrumental in maintaining the acid/alkaline pH balance in your body through the bicarbonate buffer system. This is a simple concept to understand vis-à-vis the respiratory system once you realize that when carbon dioxide dissolves in water, it can react with that water to produce carbonic acid, which acidifies the blood. This means that eliminating carbon dioxide in the blood reduces acid levels both in the blood and in the body tissue served by that blood.
Understanding what we’re trying to do when breathing is more important than it might first seem. With understanding comes the first awareness of what we can do to improve those functions.
Anatomy of the respiratory system
Surprisingly, the respiratory system and the gastrointestinal system are closely linked by evolution. Or if you prefer the shorter term perspective, the respiratory system grows out of the gastrointestinal system during the development of the fetus in the womb. This linkage can easily be seen in the shared connections in the two systems. The mouth, tongue, nasal cavities, and esophagus are involved in both respiration and eating. In fact, this linkage can at times be problematic as it puts the lungs at risk of aspiration during swallowing and vomiting.
In essence, the respiratory system consists of a series of tubes for conduction of air, then distribution of that air to the remotest corners of your lungs, and finally the exchange of gases at the capillary level. Air is inhaled through the nose and mouth, then down through the “airways,” passing from the larynx and trachea and then into a rapidly dividing series of about 23 generations of bronchi and bronchioles. The bronchi are comprised of a series of cartilaginous rings that keep them relatively rigid. But by the time you reach the smallest of the conductive tubes, the bronchioles, the cartilage is gone and the tubes are flexible — subject to opening and closing through muscle action.
In summary, the larynx, trachea, bronchi, and their smaller divisions perform pulmonary ventilation, which is simply the movement of air. The bronchioles and alveoli, which are found at the far end of the respiratory system, perform pulmonary respiration, which is the actual exchange of gases.
There are nearly 50 distinct types of cells that have been identified in the lungs — at least 12 can be found in the airways. In addition, mucus is secreted onto the surfaces of the airways by glands and by “goblet cells” abundantly present on bronchial surfaces. This mucous rests on a thin layer of an electrolyte solution and covers much of the bronchial surfaces. In addition, a large number of cells with hair like extensions called cilia can also be found along the entire length of the airways (at least in a person who doesn’t smoke). The purpose of the cilia is to capture any particles or smoke that enters the air passages, mix them with the mucous that lines the passageway, and then beat that mixture back up through the passageway until it is expelled from the lungs. From there it is either coughed and expectorated out of the body or swallowed. As a side note, approximately 500 ml of this mucous (one pint) is swallowed every day. Any damage to this system, such as that caused by smoking which destroys the cilia, leaves one prone to develop respiratory infections and bronchial dilation, which narrows the airways and restricts the ability to breathe.
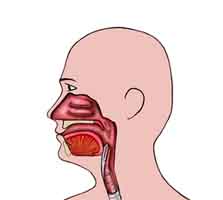 Upper airway
Upper airway
The first part of the airway (nose and mouth) is devoted to air conditioning — warming up cold air, cooling hot air, moisturizing dry air, etc. before it enters the lungs. The nasal cavity (also called the nasopharynx) is lined with mucous membranes, which contain many folds to provide a large surface area. This facilitates temperature and moisture control. It’s the reason you get a runny nose in cold air as the nasal tissue releases large quantities of fluid in an attempt to moisturize the cold dry air. In addition, the mucous produced by the membranes is thick and sticky so as to catch dust and particulate matter so it does not enter the lungs.
The epiglottis is made of cartilage and serves to prevent food or liquids from entering the lungs. When you swallow, the swallowing action causes the trachea to rise up. At the same time, the action of the tongue presses the epiglottis down on top of the trachea — thus closing off entry to the lungs. (Note: this action can be seen by watching the Adams apple which sits above the trachea and is part of the voice box as it rises up with the trachea each time you swallow.) Talking while swallowing will defeat this mechanism, leading to aspiration (the accidental sucking in of food particles or fluids into the lungs). Also, sometimes as people age, the mechanism works less efficiently, thus causing people to aspirate more and go into painful coughing fits in an attempt to force the food or liquid back out of the lungs. Major and minor episodes of aspiration contribute to the terminal stages of many diseases, and aspiration appears to play a role in a variety of chronic disorders, such as cough, bronchial asthma, bronchiectasis, and pulmonary fibrosis.
Lower airway
Like the heart, surrounded by the pericardium, the lungs are likewise enclosed in a two piece membrane called the pleura lining. This is a thin membrane which lines the inside of the chest cavity and also covers the lungs. The two “pleural cavities” (one for each lung) are enclosed compartments, with normally only a film of lubricating fluid between the layer lining the chest (parietal pleura) and the layer covering the lungs (visceral pleura).
The “visceral” layer covering the lungs is continuous with the “parietal” layer that covers the inner surface of the chest cavity — like a balloon folded over on itself. The thin layer of fluid, which separates these two layers amounts to less than 10 ml (about 1/3 of an oz) total in the normal adult lungs. This fluid contains both mesothelial cells and a significant concentration of mucopolysaccharides, which acts as a lubricant for the smooth movement of the pleural layers against one another. The two layers continually tend to pull away from each other, because of the stretched elastic condition of the lungs — an important factor in the mechanics of breathing. If the chest wall is penetrated by a wound, air is readily sucked into the pleural cavity, separating the two pleural layers and collapsing the lung.
 Air is conducted from the nose and mouth down into the lungs by the trachea (a tube made primarily of cartilage that serves only one purpose — to conduct air). At the bottom of the trachea, the passageway splits into two bronchial tubes called the mainstem bronchi — one heading into each lung. The mainstem bronchi then divide progressively into smaller and smaller segmented bronchi as they spread into the lungs. The bronchi are, like the trachea, are primarily composed of inflexible cartilage. Again, they are used for conduction of air only. At the lowest or smallest level, however, the bronchi change. The cartilage is mostly gone, and the composition is now mostly flexible muscle. These terminal bronchi are called bronchioles. As we saw with the cardiovascular system, the muscle tissue at this level allows the bronchioles to expand and contract — thus directing air flow to the different parts of the lung as needed. The whole system is known as the tracheal-bronchi tree — and it in fact looks like a tree if you turn it upside down, with the trachea serving as the trunk of the tree.
Air is conducted from the nose and mouth down into the lungs by the trachea (a tube made primarily of cartilage that serves only one purpose — to conduct air). At the bottom of the trachea, the passageway splits into two bronchial tubes called the mainstem bronchi — one heading into each lung. The mainstem bronchi then divide progressively into smaller and smaller segmented bronchi as they spread into the lungs. The bronchi are, like the trachea, are primarily composed of inflexible cartilage. Again, they are used for conduction of air only. At the lowest or smallest level, however, the bronchi change. The cartilage is mostly gone, and the composition is now mostly flexible muscle. These terminal bronchi are called bronchioles. As we saw with the cardiovascular system, the muscle tissue at this level allows the bronchioles to expand and contract — thus directing air flow to the different parts of the lung as needed. The whole system is known as the tracheal-bronchi tree — and it in fact looks like a tree if you turn it upside down, with the trachea serving as the trunk of the tree.
Note: the muscle tissue at the level of the bronchioles can sometimes present a problem. In some cases, this tissue is extremely sensitive and hyper responsive to allergens. In those cases, the muscle can lock the bronchiole in a closed state. At that point air can still be forced past the bronchiole into the alveolar sacs, but because of the constriction, it cannot leave — which makes breathing extremely difficult. This condition is known as asthma. (More on this later in the series.) Incidentally, the wheezing that asthmatics experience is merely the sound of air trying to rush through the constricted tubing.
After the division of the mainstem bronchi, each lung divides itself into three lobes — although in the left lung, the upper and middle lobes have merged together, making it look like there are only two lobes. The lobes are then divided into smaller segments named after the bronchi that go into them. From a surgical point of view, it is far easier to remove an entire lung, as opposed to just a piece of lung since you only have to staple off the one large bronchi and one main blood vessel. Lobes are also fairly easy to remove in that you are still dealing with just a handful of bronchi and blood vessels. But if you try and remove a piece of a lobe, you must close off dozens of bronchioles and blood vessels.
Exchange system
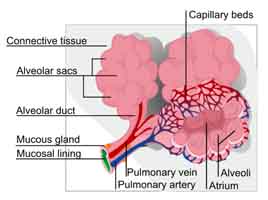 At the end of all the bronchioles are the alveoli, the microscopic air sacs that serve as the exchange system of the lungs. It is the alveoli that interact with the vast network of tiny pulmonary arterioles, venules, and capillaries — exchanging oxygen for carbon dioxide and refreshing the blood. The network of arterioles and venules literally cover the alveolar sacs complete with a spider web like network, providing access to every square inch of lung tissue. The actual exchange of gases takes place at the level of the pulmonary alveolar capillaries — the tiniest part of the system.
At the end of all the bronchioles are the alveoli, the microscopic air sacs that serve as the exchange system of the lungs. It is the alveoli that interact with the vast network of tiny pulmonary arterioles, venules, and capillaries — exchanging oxygen for carbon dioxide and refreshing the blood. The network of arterioles and venules literally cover the alveolar sacs complete with a spider web like network, providing access to every square inch of lung tissue. The actual exchange of gases takes place at the level of the pulmonary alveolar capillaries — the tiniest part of the system.
The alveoli
Alveoli begin to appear in the walls of the 17th generation of bronchioles. By the 20th generation of bronchioles, the entire wall of the airway is composed of alveoli. But the actual alveolar sacs, the bottom line of the lung so to speak, make their appearance at the 23rd generation of alveoli. There are approximately 300 million alveoli within the lungs, providing a surface area about the size of a tennis court. The barrier separating the pulmonary capillaries from the air in the alveolar sacs is composed of a layer of endothelial cells, a small interstitial space, and a layer of pulmonary epithelial cells known as pneumocytes. The exchange of oxygen for carbon dioxide in blood cells takes place across this barrier.
The tissue separating the endothelial cells and the epithelium of the lungs contains elastic, collagen fibers that give structural integrity and elasticity to the pulmonary tissues. When the chest cavity is opened, it is the elasticity of the lungs that acts to expel all of the air remaining in the lungs, which then collapse. This becomes significant when we talk about emphysema. One of the effects of emphysema is that it destroys those elastic fibers, which severely impacts the ability of the lungs to adequately contract, significantly impacting the ability of the patient to breathe. At the other end of the spectrum, however, an overgrowth of fibrous elastic tissues in the lungs happens in patients with pulmonary fibrosis and is responsible for the difficulty that they experience during inhalation — both in terms of the ability of the lungs to expand and contract and the ability of carbon dioxide and oxygen to freely pass between the pulmonary capillaries and the alveoli.
Another issue to consider is that for this system of gas exchange to work, the alveolar sacs must be composed of many, many separate alveoli so that the sac itself looks something like a bunch of grapes. The reason the multitude of alveoli is necessary is that they provide a vast surface area to accommodate the multitude of pulmonary capillaries required to “feed” the system and exchange sufficient gases. (As we mentioned a couple of paragraphs ago, in a pair of healthy lungs, the surface area is equivalent to that of a tennis court.) In some diseases, such as emphysema, the walls of the individual alveoli break down leaving you with one sack as opposed to “the bunch of grapes.” The net effect is a dramatically reduced surface area of the lungs, thereby limiting the ability of the lungs to exchange gases — thus the resulting shortness of breath. But more on this later.
It is important to note that the lungs (and for the most part we’re talking about the alveoli) are not actually hollow, but rather, sponge like. If you cut a section of the lung, it does not look like a balloon, but like a sponge. And in fact, if you squeeze the tissue, tiny little bubbles come out — just like squeezing a sponge.
It should also be noted that the alveoli are extremely susceptible to complications if any foreign particles or fluids enter them since they have no good mechanism for their removal. Pneumonia is often the end result. In fact, the defense mechanisms to prevent this are actually in the trachea and large bronchi, which, as we discussed earlier, are lined with cells that have a vast area of hair like projections called cilia that beat upwards in an attempt to move the particulate matter (including cigarette smoke, air pollution, or coal dust) out into the throat, where it can be cleared by coughing or clearing the throat. It’s probably worth mentioning that one of the first effects of smoking cigarettes or inhaling heavily polluted air is that you destroy these cilia — and thus the ability of your lungs to protect themselves from further smoking or exposure to particulate matter. Once started, it’s a vicious circle.
Diaphragm and chest wall
The last part of the respiratory system we’ll talk about is the diaphragm, which is a large, sheet-like muscle. It separates the thoracic cavity, which holds the lungs and heart, and the abdominal cavity, which holds the stomach, intestines, kidneys, and liver. Like the cavities it separates, it too is comprised of two distinct portions. The costal portion is attached to the ribs and is responsible for ventilation. The ribs meanwhile, which define the chest wall, are connected by two layers of intercostal muscles. The outer layers run diagonally downward and forward from the upper to lower ribs and act to lift the chest cavity. The internal intercostals run diagonally in the opposite direction and assist in exhalation. The scalene muscles run from the first five vertebrae to the first two ribs and lift the chest cage during inhalation.
The diaphragm is crucial for breathing and respiration. During inhalation, the diaphragm contracts, thus enlarging the thoracic cavity (the external intercostal muscles also participate in this enlargement). This reduces intra-thoracic pressure. In other words, by enlarging the chest cavity, you create suction that draws air into the lungs. When the diaphragm relaxes, air is exhaled by the elastic recoil of the lungs and the tissues lining the thoracic cavity in conjunction with the abdominal muscles, which now push inward and help the diaphragm rise up and shrink the size of the chest cavity forcing air out.
The second portion of the diaphragm consists of the crural fibers, which surround the esophagus. These fibers also contract during inhalation but have a relatively minor effect on respiration. Their primary function is that they relax when food is swallowed. The crural diaphragm also relaxes when vomiting, in contrast to the costal diaphragm, which contracts with the abdominal musculature to increase intra-abdominal pressure in an attempt to force the vomit upward — oftentimes with great force. (Think of the movie, The Exorcist.) The crural diaphragm acts in concert with the smooth muscle of the esophagus to prevent the reflux of food and gastric fluid into the esophagus.
It should also be noted that the diaphragm is involved in helping to prevent acid reflux by exerting pressure on the esophagus as it passes through the esophageal hiatus. Malfunctions here are known as hiatal hernias.
Lung facts
Like virtually all the systems and organs in our body, the lungs are a marvel of engineering and function. Awake or asleep, conscious or unconscious, our bodies breathe automatically without thought on our part.
- The normal human lungs weigh about 2 lbs or 1 kg, of which 40% to 50% is blood.
- New babies at rest breathe between 40 and 50 times per minute. By age five it decreases to around 25 times per minute.
- At rest, an adult breathes about 14 to 16 times per minute. After exercise it could increase to over 60 times per minute. Note: these rates are fixed. After years of doing yoga breathing exercises, my normal breathing rate is about six times per minute. It used to drive doctors crazy on the rare occasions I would have a physical. There are some people who believe that slowing down the rate of breathing slows down the rate of aging. I don’t know if that’s true, but after 61 years, I’d have to say, “So far so good.”
- On average, you breathe 23,000 times a day and about 600 million breaths during your lifetime.
- Each time you breathe you inhale approximately one liter of air (or up to 3 liters of air with a full inhalation). That works out to about 600,000 cubic meters (785,000 cubic yards) of air during your lifetime.
- As a side note, because you breathe so many molecules of air during your lifetime, those same molecules get shared by everyone else on the planet as they breathe. Or to look at it another way, with every breath you take, you are breathing billions of molecules of air that have previously passed through the lungs of Genghis Khan, Mary Magdalene, Albert Einstein, or Mohammed — take your pick from any name in history. It’s an amazing concept when you think about it.
Wrapping up on the anatomy of the respiratory system
Let’s take a break here. With the next issue, we’ll pick up with an exploration of the physiology of the respiratory system — how it actually works and how gases are actually exchanged. After that, we’ll move into an exploration of what can go wrong and what you can do about it. Conditions we’ll cover include:
- COPD
- Emphysema
- Asthma
- Allergies
- Bronchitis and flu
- Bird flu
- Pneumonia (can be triggered by aspiration — as happens with dolphins and whales)
- Cystic fibrosis
- Pulmonary fibrosis
- Pulmonary embolism
When we discuss those conditions, we’ll get specific as to how you can help deal with them, but for now, let’s wrap up with a look at three things you can do now to improve the health of your respiratory system.
Exercise your lungs
In my newsletter on Exercise, I talked about the importance of resistance breathing. Proper breathing is a topic worthy of its own newsletter, but for now, let’s just focus on the advantages of resistance breathing. The concept is simple: putting a device in your mouth that restricts (in a controlled manner) your inhalations and exhalations, which forces your lungs to work harder. This, in turn, strengthens the muscles that makes your lungs work and increases their capacity. There are a number of such devices widely available on the internet and in health magazines. They tend to run $20-40. The investment is well worth it since this type of exercise can significantly improve the strength of your respiratory muscles and increase your lung capacity.

How much of a benefit are we talking about?
Studies have shown that these devices can increase breathing endurance by close to 300%. Considering how fundamental oxygen is to health, it’s not hard to see the short and long-term health and performance advantages of doing so.
And for those looking to duplicate what I did with yoga breathing, the exercises I practiced were
- Kapalabhati
- Alternate nostril breathing
- Bhastrika, which you will want a teacher to guide you through
- Watching your breath. You can lie on your back for this exercise. Just visualize yourself rising and expanding with each inhalation, and floating out on the breath with each exhalation. And enjoy the spaces between the breaths. Don’t force it. Just watch. If after inhaling, you don’t feel like exhaling immediately, don’t. Just enjoy the sensation of rising and expanding. And if after exhaling, you don’t feel the need to inhale immediately, don’t. Just enjoy the sensation of floating on your breath until it’s time to inhale again. Don’t force it. Just watch and breathe.
Proteolytic enzymes
Regular use of a well designed proteolytic enzyme formula can:
- Reduce swelling of lung tissue, including the bronchioles
- Reduce allergies
- Relax and expand your bronchioles
- Thin and clear mucous from the lungs
- Help heal scars in your lung tissue
- Increase the ability of your body to utilize oxygen
Raise your pH
Although your body’s buffer systems will do everything in their power to maintain your blood’s proper pH, you can take a tremendous burden off your body and your respiratory system in particular in accomplishing this task by taking alkalinizing supplements or treated water to raise your pH. You have a number of options including, but not limited to:
- Alkalinizing drops — for example
- Alkaline trace minerals — for example
- Water ionizer — for example
And that’s it for now. We’ll pick up in the next issue with an examination of the physiology of the respiratory system.
For more information on the Respiratory System:












Great reading very
Great reading very informative, my partner has chronic respiratory problems , allergies etc I am embarking on a journey to help him as yet for some reason he has not done it, to improve his respiratory and lungs, as every year he has a upper respiratory infection effecting his lungs. Takes him ages to recover. Can you please advise me, do you have newsletter I could join. What do you feel I should do and should we see lung consultant. He would be happy to do that and other things.
Many thanks Fiona
Hi Fiona,
Hi Fiona,
I would just do a search on our site for all the articles we have on this topic, and make sure to check out the Health Topics section (link above). Our newsletter and daily health tip are also great, sign up form is on the right hand side of this page (top) or just click here: http://www.jonbarron.org/free-downloads
Valuable info. Lucky me I
Valuable info. Lucky me I found your website by accident, and I’m shocked why this accident didn’t happened earlier! I bookmarked it.
Very useful. Thanks for this!
Very useful. Thanks for this! I am saying this because it is helping me in an assignment in Science that is about the Respiratory System, Beautiful Timing!
😀