Sperm counts have been trending downwards for decades. Women are becoming less fertile. And a new study now suggests that we might be approaching the threshold of mass infertility in men and the possible extinction of the human race. Well, there’s no way to sugar coat it; it’s all true. Well, maybe not the mass extinction part. But don’t despair. Although you can’t do anything about how things are trending, you can take steps to move yourself off the trendline and maintain your fertility as others all around are losing theirs. But first let’s look at the study that was recently released, producing a wave of dire headlines in the mainstream media.
“Men’s sperm count drops dramatic 52 percent.” The Washington Times. 1 Renee Garfinkel. “Men’s sperm count drops dramatic 52 percent.” The Washington Times. August 7, 2017. (Accessed 15 Aug 2017.) http://www.washingtontimes.com/news/2017/aug/7/male-sperm-count-drops-dramatically-west/
“Worldwide Sperm Counts Are Dropping at an Alarming Rate.” big think.2 ROBBY BERMAN. “Worldwide Sperm Counts Are Dropping at an Alarming Rate.” big think. August 8, 2017. (Accessed 15 Aug 2017.) http://bigthink.com/robby-berman/worldwide-sperm-counts-are-dropping-at-an-alarming-rate
“DOES A DECLINING SPERM COUNT SPELL THE END OF HUMANITY?” Newsweek.3 RONALD BAILEY. “DOES A DECLINING SPERM COUNT SPELL THE END OF HUMANITY?” Newsweek. 8/6/17. (Accessed 15 Aug 2017.) http://www.newsweek.com/does-declining-sperm-count-spell-end-humanity-646640
“Huge Drop in Sperm Count Could Be Next Cause of Human Extinction.” The Christian Post.4 Felix N. Codilla III. “Huge Drop in Sperm Count Could Be Next Cause of Human Extinction.” The Christian Post. Aug 4, 2017. (Accessed 15 Aug 2017.) http://www.christianpost.com/news/huge-drop-in-sperm-count-could-be-next-cause-of-human-extinction-194200/
Temporal Trends in Sperm Count: A Systematic Review and Meta-Regression Analysis
The first thing to understand is that this is not a new, double-blind study, but rather a retrospective analysis of 185 previously conducted academic studies (whittled down from an initial pool of 7,518 relevant publications) that collected data from men around the world over a 40-year period. And according to the analysis, sperm counts around the world have been declining steadily over the last four decades–to the point that current sperm counts are less than half of what they were 40 years ago.5 Hagai Levine, Niels Jørgensen, Anderson Martino-Andrade, et al. “Temporal trends in sperm count: a systematic review and meta-regression analysis.” Human Reproduction Update, pp. 1–14, 2017. http://academic.oup.com/humupd/article/doi/10.1093/humupd/dmx022/4035689/Temporal-trends-in-sperm-count-a-systematic-review Specifically, between 1973 and 2011, sperm counts have declined 59.3%. And if that’s not bad enough, there is “no evidence” that this decline has leveled off in recent years. All evidence points to the fact that sperm counts have continued to decline since 2011–and are continuing to decline even as you read this.
Things get even more interesting when you dig deeper and realize that declines are significant only in studies from North America, Europe, Australia (and New Zealand), where they are most pronounced among men unselected by fertility. In this latter group, sperm concentration (SC) declined 52.4% (−1.4% per year) and total sperm count (TSC) 59.3% (−1.6% per year) over the study period. These slopes remained substantially unchanged after controlling for multiple variables such as age, abstinence time, method of semen collection, method of counting sperm, selection of population and study exclusion criteria, number of samples per man, and completeness of data–and in multiple sensitivity analyses. To translate: these data provide a robust indication for a decline in Sperm Concentration and Total Sperm Count in North America, Europe, Australia and New Zealand over the last 4 decades. And once again, there is no sign of the decline ‘leveling off,’ even when analyses are restricted to sample collection in the last five years of the analysis. As the researchers pointed out, “Declining mean sperm count implies that an increasing proportion of men have sperm counts below any given threshold for sub-fertility or infertility. The high proportion of men from western countries with concentration below 40 million/ml is particularly concerning given the evidence that sperm count below this threshold is associated with a decreased monthly probability of conception.6 Bonde JP, Ernst E, Jensen TK, et al. “Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners.” Lancet 1998;352: 1172–1177. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(97)10514-1/abstract
Dr. Hagai Levine, the lead researcher on the study, said the findings left him feeling “very worried.” He pointed to environmental factors such as the exposure to pesticides and chemicals (both xenoestrogens), lifestyle habits like smoking and poor diet, and psychological factors such as stress as potential causes for the steep decline in sperm count.
And keep in mind that declines in sperm count have implications beyond fertility and reproduction. The decline reported in this analysis is consistent with reported trends in other male reproductive health indicators, such as testicular germ cell tumors, cryptorchidism (undescended testicles), onset of male puberty, and total testosterone levels.7 Skakkebaek NE, Rajpert-De Meyts E, Buck Louis GM, et al. “Male reproductive disorders and fertility trends: influences of environment and genetic susceptibility.” Physiol Rev 2016;96:55–97. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698396/ And beyond that, recent studies have shown that poor sperm count is associated with overall morbidity and mortality.8 Jensen TK, Jacobsen R, Christensen K, Nielsen NC, Bostofte E. “Good semen quality and life expectancy: a cohort study of 43,277 men.” Am J Epidemiol 2009;170: 559–565. http://academic.oup.com/aje/article/170/5/559/102217/Good-Semen-Quality-and-Life-Expectancy-A-Cohort , 9 Eisenberg ML, Li S, Behr B, Cullen MR, et al. “Semen quality, infertility and mortality in the USA.” Hum Reprod. 2014 Jul; 29(7): 1567–1574. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4059337/ , 10 Eisenberg ML, Li S, Cullen MR, Baker LC. “Increased risk of incident chronic medical conditions in infertile men: analysis of United States claims data.” Fertil Steril 2016; 105:629–636. http://www.fertstert.org/article/S0015-0282(15)02087-7/fulltext , 11 Latif T, Kold Jensen T, Mehlsen J, et al. “Semen quality is a predictor of subsequent morbidity. A Danish cohort study of 4,712 men with long-term follow-up.” Am J Epidemiol 11.05.2017. http://academic.oup.com/aje/article-abstract/doi/10.1093/aje/kwx067/3814531/Semen-Quality-as-a-Predictor-of-Subsequent While the current study was not designed to provide direct information on the causes of the observed declines, sperm count has been plausibly associated with multiple environmental and lifestyle influences, both prenatally and in adult life. In particular, endocrine disruption from chemical exposures or maternal smoking during critical windows of male reproductive development may play a role in prenatal life (however, with smoking rates going down in most Western countries, that would indicate that chemical exposure was more likely to be culpable in the ongoing increases). And lifestyle changes and exposure to xenoestrogens in the form of pesticides and phthalates also probably play a role in adult life. And as the report concluded, “Thus, a decline in sperm count might be considered as a ‘canary in the coal mine’ for male health across the lifespan. Our report of a continuing and robust decline should, therefore, trigger research into its causes, aiming for prevention.”
When all is said and done, the consequences for humanity, if not yet apocalyptic, are certainly very, very disturbing. Quite simply, this study implies that a growing number of men have sperm counts that are already below the thresholds for either reduced fertility or full-fledged infertility. And this is not theoretical. As Dr. Levine said, “Eventually we may have a problem, and with reproduction in general,” he told the BBC. “And it may be the extinction of the human species.”
Fertility Rates in the US and Around the World
Now, before we begin to panic, we would need to see evidence of related problems in other aspects related to the reproductive chain–fertility rates being an obvious one. If sperm counts are indeed already dancing on the edge of viability, then we should see cracks beginning to appear in fertility data.
The general fertility rate gives an idea of how many children are being born into the population during a specific period. These numbers can be monitored to assess levels of reproduction within a population over time. When it comes to births, it tells us about future members of society that will go on to replace the current workforce and will be generating tax revenues, supporting the older generations, and so on.
Well, according to a report just released by the CDC’s National Center for Health Statistics on August 8, 2017, the US fertility rate has dropped to the lowest level ever seen since fertility records started being kept more than a century ago.12 Rossen LM, Osterman MJK, Hamilton BE, Martin JA. “Quarterly provisional estimates for selected birth indicators, 2015-Quarter 1, 2017.” National Center for Health Statistics. National Vital Statistics System, Vital Statistics Rapid Release Program. August 8, 2017. (Accessed 12 Aug 2017.) http://www.cdc.gov/nchs/products/vsrr/natality-dashboard.htm# And it’s not just noticeable as a long-term trend, which it is. But the report makes clear that even just the shift from last year to this year, taken by itself, is significant.
Not to worry, though. According to Brady Hamilton, a statistician-demographer with the center and one of the report’s authors, it is important to remember that although the country is at record lows in fertility, there is also a large influx of immigrants to offset the decline in fertility. Then again, upcoming political decisions about immigration levels could render Hamilton’s comment moot. The bottom line is that fewer young people means fewer workers to support a growing cohort of retirees, adding strains to pension and health care systems. In other words, before we worry about the mass extinction of humanity, we may have to deal with the collapse of social contract as we know it.
Likewise, in Europe, fertility levels have dropped precipitously over the last half century, although they have shown signs of stabilizing over the last 10 years–albeit at unsustainable levels.13 “Fertility Statistics.” Eurostat. March 2017. (Accessed 12 Aug 2017.) http://ec.europa.eu/eurostat/statistics-explained/index.php/Fertility_statistics Again, as with the US, they will require an influx of immigrants to sustain their productivity and tax base–but only if those immigrants integrate into the workforce and tax base. If they don’t, it merely exacerbates the problem.
And in Japan, things are several degrees worse. Deaths have outpaced births for several years. After Japan’s population hit a peak of 128 million at the start of the current decade, it shrank by close to 1 million in the five years through 2015, according to census data. By itself, that might not sound too dire, but demographers expect it to plunge by an astonishing one-third by 2060, to as few as 80 million people — a net loss of 1 million a year, on average. Last year, in fact, according to the Japanese Ministry of Health, Labour and Welfare, the number of births in Japan dropped below one million for the first time.14 Jonathan Sobel. “Japan, Short on Babies, Reaches a Worrisome Milestone.” New York Times. June 2, 2017. (Accessed 12 Aug 2017.) http://www.nytimes.com/2017/06/02/business/japan-population-births.html The shrinking of the country’s population is already affecting job and housing markets, consumer spending, and long-term investment plans at businesses. Again, with fewer young people to maintain the economy and provide for senior citizens, it could ultimately mean the end of Japanese society as we know it.
Now, to be sure, much of this drop in fertility rates represents a conscious choice by citizens in wealthy countries to have fewer children. But not all of it. And more importantly, at some point in the future, if the population in a given country decides that they want more kids, but if sperm counts and female fertility have dropped into full-fledged infertility, having a choice at that point may be moot.
But as with declining sperm counts, there are too many unknowns related to fertility rates to draw any clear conclusions. We need more, and we may have that in the incidence of cryptorchidism that we mentioned earlier.
Cryptorchidism
Cryptorchidism is the failure of one or both testes to descend into the scrotum prenatally. It currently occurs in 2.4%–5% of newborns.15 Fatma Fawzy,1 Amr Hussein,2 Mostafa Mahmoud Eid, et al. “Cryptorchidism and Fertility.” Clin Med Insights Reprod Health. 2015; 9: 39–43. Clin Med Insights Reprod Health. 2015; 9: 39–43. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4689328/ Many of these testes will descend spontaneously shortly after birth, but ~23% will remain undescended unless surgery is performed. Men born with both testicles undescended have a six times greater risk of being infertile when compared with unilaterally cryptorchid men and the general male population. Approximately 10% of infertile men have a history of cryptorchidism and orchidopexy (the surgical procedure used to correct it). The main reasons for infertility in men with a history of cryptorchidism treated by surgery are maldevelopment of the testes and an improper environment for the normal development of the testes, hyperthermia (don’t wear tighty whities, by the way), and anti-sperm antibodies.
Now, here’s the key point when it comes to cryptorchidism. Although only a few reliable studies have been performed to evaluate trends in cryptorchidism incidence, and it is also difficult to compare data derived from different countries because of the lack of precise methodology, the bottom line is that the great majority of published data all point to an increase in the incidence of cryptorchidism over recent decades in North America and Europe.16 Thonneau, Patrick F., Candia, Peggy, Mieusset, Roger. “Cryptorchidism: Incidence, Risk Factors, and Potential Role of Environment; An Update.” Journal of Andrology Volume 24, Issue 2. March-April 2003. Pages 155–162. http://onlinelibrary.wiley.com/doi/10.1002/j.1939-4640.2003.tb02654.x/full
The incidence of cryptorchidism is indeed increasing. And yes, some studies have indicated that some of this increase may be due to advances in screening resulting in the detection of potential cases that might have been missed in the past.17 Brucker-Davis F, Pointis G, Chevallier D, Fenichel P. “Update on cryptorchidism: endocrine, environmental and therapeutic aspects.” J Endocrinol Invest. 2003;26(6):575–587. http://www.ncbi.nlm.nih.gov/pubmed/12952375 But these same studies acknowledge that other male reproductive problems, such as subfertility, hypospadias (an incorrectly located urethra), and testicular cancer appear to also be on the increase–and that can’t be explained away by improved observation. In fact, according to most researchers, this trend suggests the possible in utero impact of hormonally active environmental factors, such as pesticides with estrogenic or testosterone blocking effect. Not surprisingly, then, it is consistent with the increased risk of cryptorchidism observed in the sons of mothers exposed to diethylstilbestrol (a synthetic estrogen once used during pregnancy–with disastrous effect–to prevent miscarriages). The bottom line is that environmental factors are likely to be a potential cause of the increased incidence of cryptorchidism recently. This is further supported by the finding that the increased incidence of cryptorchidism has been mainly noticed in industrial countries where exposure to harmful environmental materials is expected to be more.
The case is now starting to build. Reduced sperm count, lowered fertility, and cryptorchidism all share one thing in common: exposure to synthetic estrogens. We may not have a smoking gun yet, but things certainly are starting to get warm. But is there more?
Puberty in Girls
In girls, puberty is commonly defined as breast development, growth of pubic hair and menarche, the beginning of the menstrual cycle. At the turn of the 20th century, the average age for an American girl to get her period was 16 to 17. Today, that number has plummeted to as young as 8 or 9. More astonishing, at age three, 3% of African-American girls and 1% of Caucasian girls show breast and/or pubic hair development.18 Kaplowitz, P.B., S.E. Oberfield, and the Drug and Therapeutics and Executive Committees of the Lawson Wilkins Pediatric Endocrine Society. “Reexamination of the Age Limit for Defining When Puberty is Precocious in Girls in the United States: Implications for Evaluation and Treatment.” Pediatrics 104:4 (October 1999): 936–941. http://pediatrics.aappublications.org/content/104/4/936 , 19 Herman-Giddens, M.E., E.J. Slora, R.C. Wasserman, et al. “Secondary Sexual Characteristics and Menses in Young Girls Seen in Office Practice: A Study from the Pediatric Research in Office Settings Network.” Pediatrics 99:4 (1997): 505–512. http://www.researchgate.net/publication/14123686_Secondary_Sexual_Characteristics_and_Menses_in_Young_Girls_Seen_in_Office_Practice_A_Study_from_the_Pediatric_Research_in_Office_Settings_Network
Among the toxins causing this trend, the biggest offenders are plastic compounds, in particular, phthalates, 20 Colón I1, Caro D, Bourdony CJ, Rosario O. “Identification of phthalate esters in the serum of young Puerto Rican girls with premature breast development.” Environ Health Perspect. 2000 Sep;108(9):895-900. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2556932/pdf/ehp0108-000895.pdf man-made xenoestrogens found all over the place: in plastic food and beverage containers, carpeting, shampoos, insect repellents, vinyl flooring, shower curtains, plastic toys, and in the steering wheels and dashboards of most cars. Our bodies cannot metabolize phthalates, which directly interfere with the endocrine system–the body’s system of glands and hormones–and harm fat cells. Indirectly, phthalates may cause weight gain, which can by itself speed up the timing of puberty.
To be sure, the phytoestrogens in soy formula and soy milk consumed to excess are likely to play a role, but, once again, we find xenoestrogens as a common thread in yet another reproductive crisis. So, what exactly are xenoestrogens?
Xenoestrogens
Xeno is ancient Greek for “stranger or foreign,” so xenoestrogens can be translated as “foreign estrogens”–that is, coming from outside the human body. Xenoestrogens can mimic our body’s estrogen hormones, attaching to estrogen receptor sites in our bodies. They interfere with our natural estrogens; disrupt hormone balance and menstrual cycles, affect prostate health, contribute to problems with fibroids, endometriosis, uterine cysts, and polycystic ovary syndrome, and can damage ova and sperm. Many xenoestrogens activate the CYP-lBl enzyme, which converts our body’s naturally occurring estrogens to 4 catechols, a toxic estrogen that can damage the body’s DNA and increase the risk of developing cancer, including breast cancer.
The problem we face today is that industry has dumped untold numbers of untested endocrine disruptors into our environment. They are everywhere, and they are inescapable. And even if we immediately halted the release of all disruptors into the environment from this moment forward (something not even close to happening), it would take several generations–several lifetimes, if you will–for them to clear the planet. The bottom line is that we are going to have to live with them and their consequences far into the future.
So, what exactly are these endocrine disruptors?
Xenoestrogens are mostly–but not exclusively–petroleum-based synthetic estrogens that are close enough in molecular structure to natural estrogen that they can bind to estrogen receptor sites with potentially hazardous outcomes. They are now present in massive amounts in our food chain, water supply, and environment. Xenoestrogen contamination has been identified as a major source of deficient sperm quality. In fact, xenoestrogens effect damage at both the hypothalamo-pituitary level and on testicular spermatogenesis. Even worse, not only are xenoestrogens omnipresent, they are considerably more potent than estrogen made by the ovaries–some are even potent in amounts as small as a billionth of a gram. Sources of xenoestrogens include plastics, pesticides, chemicals, and water systems.
As many anthropogenic agents (pollution deriving from human activity) are xenoestrogens, environmental health research has focused on estrogen receptor level disturbances and on aromatase abnormalities in the genetic code. Cancer types that have been well documented in literature to be related with environmental exposure include the reproductive system, breast, lung, kidney, pancreas, and brain. Research has shown both a significant correlation between exposure to xenoestrogens and increased, gender-related, cancer risk. It would make sense, then, to re-evaluate agents so far defined as endocrine disruptors, as they are also key molecules in carcinogenesis.21 Aleksandra Fucic, Marija Gamulin,Zeljko Ferencic, et al. “Environmental exposure to xenoestrogens and oestrogen related cancers: reproductive system, breast, lung, kidney, pancreas, and brain.” Environ Health. 2012; 11(Suppl 1): S8. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3388472/
Now that we understand what they are, let’s look at some of the specific xenoestrogens that are adversely affecting us–in terms of everything from flagging sperm counts to early puberty in girls to multiple forms of cancer.
BPA
Bisphenol A (BPA) is an endocrine disrupting environmental contaminant used in a wide variety of products. In 2011, an estimated 10 billion pounds of BPA were produced for manufacturing polycarbonate plastic, making it one of the highest volume chemicals produced in the world.22 vom Saal FS, Nagel SC, Benjamin L, et al. “The estrogenic endocrine disrupting chemical bisphenol A (BPA) and obesity”. Molecular and Cellular Endocrinology. Environment, Epigenetics and Reproduction 354 (1–2): 74–84. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306519/ Its metabolites are found in almost everyone’s urine, suggesting widespread exposure from multiple sources. Regulatory agencies estimate that virtually all BPA exposure is from food and beverage packaging, but that’s not entirely honest. It’s also applied to the outer layer of thermal receipt paper at high levels–as a print developer–which means it gets all over your hands. Combine that with the use of hand sanitizers and skincare products that contain skin penetration agents, and you can increase absorption of BPA through the skin a hundredfold. And as we’ve discussed in previous newsletters, it’s so-called “safer” replacements BPS and BPF are not any safer and might be even worse.
Phthalates
Phthalates are any of various salts or esters of phthalic acid. They are used in personal care products and used to soften and increase the flexibility of plastics and polyvinyl chloride (PVC). Like BPA, phthalates are considered stealth chemicals unsuspectingly found in so many things we use every day including plastic food containers, beverage containers, plastic wrap, cosmetics, air fresheners, insecticides, building materials, cars, clothing, toys, electronics, medical devices, and even plastic jewelry–especially children’s jewelry. Studies have linked phthalates to hormone changes, lower sperm count, less mobile sperm, birth defects in the male reproductive system, obesity, diabetes and thyroid irregularities. And if that’s not enough, studies have shown that they can cause testicular cell death.
PCBs (products made with polychlorinated biphenyl)
Because of PCBs environmental toxicity, its classification as a persistent organic pollutant, and being a known carcinogen, its production was banned by the United States Congress in 1979 and by the Stockholm Convention on Persistent Organic Pollutants in 2001. Unfortunately, prior to the ban in 1979, PCBs entered the air, water, and soil during manufacture and use. Wastes from the manufacturing process that contained PCBs were often placed in dump sites or landfills. Occasionally, accidental spills and leaks from these facilities or transformer fires could result in PCBs entering the environment. So, even though its use has been banned for almost 40 years, it’s still omnipresent. Many rivers and buildings including schools, parks, and other sites are contaminated with PCBs, and there have been contaminations of food supplies with the toxins.
Dioxins
Dioxins are a class of several hundred toxic compounds that share certain chemical structures and biological characteristics. There are essentially three groups of dioxins.
- Chlorinated dibenzo-p-dioxins (CDDs),
- Chlorinated dibenzofurans (CDFs) and
- Certain polychlorinated biphenyls (PCBs).
CDDs and CDFs are not created intentionally, but are produced as a result of human activities like industrial bleaching and the backyard burning of trash. Natural processes like forest fires also produce CDDs and CDFs. PCBs, as we just discussed above, are manufactured products, but they are no longer produced in the United States. Nevertheless, they are still present in the environment. Again, dioxin is not produced or used commercially in the United States. It is a contaminant formed in the production of some chlorinated organic compounds, including a few herbicides. Most of the current exposures to dioxins in the US is due to releases that occurred decades ago. More than 90% of human exposure is through food, mainly meat and dairy products, fish, and shellfish.
Dioxins are highly toxic and can cause cancer, reproductive and developmental problems, damage to the immune system, and can interfere with hormones. Specifically, dioxins can disrupt both male and female sex hormone signaling in the body. Recent research has shown that exposure to low levels of dioxin in the womb and early in life can both permanently affect sperm quality and lower the sperm count in men during their prime reproductive years23 Gray LE Jr, Kelce WR, Monosson E, Ostby JS, Birnbaum LS. “Exposure to TCDD during development permanently alters reproductive function in male Long Evans rats and hamsters: reduced ejaculated and epididymal sperm numbers and sex accessory gland weights in offspring with normal androgenic status.” Toxicol Appl Pharmacol. 1995 Mar;131(1):108-18. http://www.ncbi.nlm.nih.gov/pubmed/7878665 as well as impact female fertility for several generations.24 Kaylon L.Bruner-Tran, Kevin G.Osteen. “Developmental exposure to TCDD reduces fertility and negatively affects pregnancy outcomes across multiple generations?.” Reproductive Toxicology Volume 31, Issue 3, April 2011, Pages 344-350. http://www.sciencedirect.com/science/article/pii/S089062381000314X But that’s not all! Dioxins are very long-lived, build up over decades in both the water supply and food chain–thus, ultimately in the body.
Atrazine
Atrazine is an organic compound widely used as an herbicide. Its use is controversial due to widespread contamination in drinking water and its association with birth defects and menstrual problems when consumed by humans at concentrations below government standards. Although it has been banned in the European Union, it is still one of the most widely used herbicides in the world. Atrazine is suspected of causing demasculinization in male northern leopard frogs even at low concentrations and of being an estrogen disruptor.25 Tyrone Hayes, Kelly Haston, Mable Tsui, et al. “Atrazine-Induced Hermaphroditism at 0.1 ppb in American Leopard Frogs” Environmental Health Perspectives. 111 (4): 568–75. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1241446/ A 2010 study found that exposure to atrazine caused complete feminization and chemical castration in male African clawed frogs.26 Hayes TB, Khoury V, Narayan A, et al. “Atrazine induces complete feminization and chemical castration in male African clawed frogs (Xenopus laevis).” Proc Natl Acad Sci U S A. 2010 Mar 9;107(10):4612-7. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2842049/ It has also been linked to breast tumors, delayed puberty and prostate inflammation in animals, and some research has linked it to prostate cancer in humans.
Atrazine is the main weapon against weeds in the growing of sweet corn, with few alternatives.27 University of Illinois College of Agricultural, Consumer and Environmental Sciences. “Atrazine is the main weapon against weeds in sweet corn, with few alternatives.” ScienceDaily. 5 May 2010. www.sciencedaily.com/releases/2010/05/100505102609.htm As a result, it’s a pervasive drinking water contaminant.
Organophosphate pesticides
Organophosphates (OP) are among the most commonly used of all pesticides. The research by American companies that led to the development of these pesticides was based on original research done by the Nazis in WWII to create nerve gases such as Sarin, Tabun, and Soman. Now, organophosphates form the basis for many pesticides and herbicides, and they’re also used as solvents and plasticizers. They work by irreversibly inactivating an enzyme called acetylcholinesterase, which is essential to nerve function in humans, insects, and animals. While organophosphates replaced an earlier class of compounds called organochlorides (including DDT) because they degrade more quickly, OPs have a far higher level of toxicity.
Although they are most cited for their effects on brain development, studies have shown that they do affect fertility as well. In one study, 31 men who were exposed to OP pesticides were examined just one day after exposure. Semen analysis revealed a significant reduction of semen volume and an increase in semen pH in men with OP metabolites.28 Yucra, Sandra, Gasco, Manuel, Rubio, Julio. et al. “Semen quality in Peruvian pesticide applicators: association between urinary organophosphate metabolites and semen parameters.” Environmental Health 2008 7:59. http://ehjournal.biomedcentral.com/articles/10.1186/1476-069X-7-59 In addition, multiple regression analysis showed that both occupational exposure to pesticides and the time of exposure to pesticides were more closely related to alterations in semen quality parameters than the single measurement of OP metabolites in urine.
Perfluorinated chemicals (PFCs)
Perfluorinated compounds (PFCs) are everywhere. These man-made chemicals are used in a plethora of household items, including our clothing, food packaging, non-stick cookware, and carpeting, to name just a few. They may make life a little easier, since they are designed to prevent stains and sticking, but now research is finding that this convenience may come at a high price.
PFOA (perfluorooctanoic acid), one of the more common PFCs, persists indefinitely in the environment. It is a toxicant and carcinogen in animals. PFOA has been detected in the blood of more than 98% of the general US population, with higher levels in chemical plant employees and surrounding subpopulations. Exposure has been associated with increased cholesterol and uric acid levels, and recently higher serum levels of PFOA were found to be associated with increased risk of chronic kidney disease in the general United States population, consistent with earlier animal studies. And yes, PFOA has been associated with compromised semen quality and reproductive hormone levels in men29 Vested A, Ramlau-Hansen CH, Olsen SF, et al. “Associations of in utero exposure to perfluorinated alkyl acids with human semen quality and reproductive hormones in adult men.” Environ Health Perspect. 2013 Apr;121(4):453-8. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3620740/ as well as reduced female fertility.30 Fei C, McLaughlin JK, Lipworth L, Olsen J. “Maternal levels of perfluorinated chemicals and subfecundity.” Hum Reprod. 2009 May;24(5):1200-5. http://www.ncbi.nlm.nih.gov/pubmed/19176540
Glycol Ethers
Glycol ethers are solvents found in pharmaceuticals, sunscreens, cosmetics, inks, dyes and water based paints, as well as degreasers, cleaners, aerosol paints and adhesives. Although generally considered “non-toxic,” they have been associated with low motile sperm counts31 Nicola Cherry, Harry Moore, Roseanne McNamee,et al. “Occupation and male infertility: glycol ethers and other exposures”. Occup. Environ. Med. 65 (10): 708–714. http://www.ncbi.nlm.nih.gov/pubmed/18417551 , 32 Welch LS, Schrader SM, Turner TW, Cullen MR. “Effects of exposure to ethylene glycol ethers on shipyard painters: II. Male reproduction.” Am J Ind Med. 1988;14(5):509-26. http://www.ncbi.nlm.nih.gov/pubmed/3228067 and shrunken testicles.33 Nagano K, Nakayama E, Koyano M, et al. “Testicular atrophy of mice induced by ethylene glycol mono alkyl ethers (author’s transl).” Sangyo Igaku. 1979 Jan;21(1):29-35. http://www.ncbi.nlm.nih.gov/pubmed/470211 Non-toxic indeed!
Other Endocrine Disruptors
There are certainly other endocrine disruptors including fire retardants, perchlorates, and heavy metals such as lead, mercury, and arsenic. But their effect tends to be on organs outside of the reproductive system, such as the thyroid and brain. So, although they are important, a discussion of their toxicity lies outside of the parameters of today’s discussion.
Conclusion
So, are we at reproductive Armageddon yet? No, of course not. The facts on the ground tell us that people are still having babies. Much of the drop in fertility rates is by choice–as couples get married later in life and women choose careers over family. Or married couples, for that matter, just choose to have fewer children. But!! What is choice now may not be a choice in the not so distant future. As Dr. Levine said, “Eventually we may have a problem, and with reproduction in general. And it may be the extinction of the human species.”
Now, to be sure, that’s likely to prove overly dramatic. Even if sperm counts drop below the viability threshold, in vitro fertilization could make up the difference–at least for a while. However, we may face a “momentum” problem. Things may have been set in motion that may very well continue in an unfavorable direction, even if we instantly stopped dumping any more endocrine disruptors into the environment. Remember, some of those disruptors never degrade and will continue to leach into the environment for decades to come–steadily increasing their concentration in our food supply and drinking water–and thus, ultimately, our bodies. In other words, ever higher exposure and the risk of ever higher concentrations in the body may very well be inevitable no matter what actions we take as a society today–in the unlikely event we decided to act today. And as we know from the Toxic Nation study, even if you live hundreds of miles away from the sources of pollution and live a pure organic lifestyle, you’re still going to accumulate toxins at an alarming rate.
At first glance, that’s a grim prognosis. Is there anything we can do? And the answer is: yes! Although you may not be able to stop the pollution going forward or the toxins entering your body, there are things you can do to slow things down, even clean out toxins once they’ve entered your body, or counter the ones that remain.
- Use a water filter. It will at least remove the endocrine disruptors from your drinking water. You still, of course, must deal with those disruptors in your food supply and those entering your body through your skin, but eliminating one source is better than nothing.
- Eat organic. It doesn’t guarantee that your food is xenoestrogen free, but it certainly improves the odds that it contains less.
- Lose weight. Most endocrine disruptors love to hide in your fat cells. The heavier you are, the more xenoestrogens you store.
- Fast regularly. Autolysis guarantees that the cells your body eliminates when you fast are the ones that contain the most toxins.
- Detox regularly–every three months so that you cycle through two full-body detoxes (intestinal, heavy metal, kidney, liver/gallbladder, and blood) a year. Detoxing can remove a major chunk of the endocrine disruptors.
- Incorporate foods that contain weak phytoestrogens to block estrogen receptor sites so they are unavailable to xenoestrogens. This includes foods such as soybeans and soy products (in moderation), flaxseeds, oats, barley, lentils, sesame seeds, yams, alfalfa, and apples.
- And finally, use a progesterone crème (either a women’s or men’s formula) regularly. Progesterone actively counters xenoestrogens–blocking receptor sites throughout the body so they can’t access them.
If things keep moving in the same direction, then Dr. Levine’s concerns about the extinction of the human race may become reality. But until that time several generations in the future, anyone alive today who follows the seven steps outlined above should avoid that fate and produce all the children they want.
References
| ↑1 | Renee Garfinkel. “Men’s sperm count drops dramatic 52 percent.” The Washington Times. August 7, 2017. (Accessed 15 Aug 2017.) http://www.washingtontimes.com/news/2017/aug/7/male-sperm-count-drops-dramatically-west/ |
|---|---|
| ↑2 | ROBBY BERMAN. “Worldwide Sperm Counts Are Dropping at an Alarming Rate.” big think. August 8, 2017. (Accessed 15 Aug 2017.) http://bigthink.com/robby-berman/worldwide-sperm-counts-are-dropping-at-an-alarming-rate |
| ↑3 | RONALD BAILEY. “DOES A DECLINING SPERM COUNT SPELL THE END OF HUMANITY?” Newsweek. 8/6/17. (Accessed 15 Aug 2017.) http://www.newsweek.com/does-declining-sperm-count-spell-end-humanity-646640 |
| ↑4 | Felix N. Codilla III. “Huge Drop in Sperm Count Could Be Next Cause of Human Extinction.” The Christian Post. Aug 4, 2017. (Accessed 15 Aug 2017.) http://www.christianpost.com/news/huge-drop-in-sperm-count-could-be-next-cause-of-human-extinction-194200/ |
| ↑5 | Hagai Levine, Niels Jørgensen, Anderson Martino-Andrade, et al. “Temporal trends in sperm count: a systematic review and meta-regression analysis.” Human Reproduction Update, pp. 1–14, 2017. http://academic.oup.com/humupd/article/doi/10.1093/humupd/dmx022/4035689/Temporal-trends-in-sperm-count-a-systematic-review |
| ↑6 | Bonde JP, Ernst E, Jensen TK, et al. “Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners.” Lancet 1998;352: 1172–1177. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(97)10514-1/abstract |
| ↑7 | Skakkebaek NE, Rajpert-De Meyts E, Buck Louis GM, et al. “Male reproductive disorders and fertility trends: influences of environment and genetic susceptibility.” Physiol Rev 2016;96:55–97. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698396/ |
| ↑8 | Jensen TK, Jacobsen R, Christensen K, Nielsen NC, Bostofte E. “Good semen quality and life expectancy: a cohort study of 43,277 men.” Am J Epidemiol 2009;170: 559–565. http://academic.oup.com/aje/article/170/5/559/102217/Good-Semen-Quality-and-Life-Expectancy-A-Cohort |
| ↑9 | Eisenberg ML, Li S, Behr B, Cullen MR, et al. “Semen quality, infertility and mortality in the USA.” Hum Reprod. 2014 Jul; 29(7): 1567–1574. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4059337/ |
| ↑10 | Eisenberg ML, Li S, Cullen MR, Baker LC. “Increased risk of incident chronic medical conditions in infertile men: analysis of United States claims data.” Fertil Steril 2016; 105:629–636. http://www.fertstert.org/article/S0015-0282(15)02087-7/fulltext |
| ↑11 | Latif T, Kold Jensen T, Mehlsen J, et al. “Semen quality is a predictor of subsequent morbidity. A Danish cohort study of 4,712 men with long-term follow-up.” Am J Epidemiol 11.05.2017. http://academic.oup.com/aje/article-abstract/doi/10.1093/aje/kwx067/3814531/Semen-Quality-as-a-Predictor-of-Subsequent |
| ↑12 | Rossen LM, Osterman MJK, Hamilton BE, Martin JA. “Quarterly provisional estimates for selected birth indicators, 2015-Quarter 1, 2017.” National Center for Health Statistics. National Vital Statistics System, Vital Statistics Rapid Release Program. August 8, 2017. (Accessed 12 Aug 2017.) http://www.cdc.gov/nchs/products/vsrr/natality-dashboard.htm# |
| ↑13 | “Fertility Statistics.” Eurostat. March 2017. (Accessed 12 Aug 2017.) http://ec.europa.eu/eurostat/statistics-explained/index.php/Fertility_statistics |
| ↑14 | Jonathan Sobel. “Japan, Short on Babies, Reaches a Worrisome Milestone.” New York Times. June 2, 2017. (Accessed 12 Aug 2017.) http://www.nytimes.com/2017/06/02/business/japan-population-births.html |
| ↑15 | Fatma Fawzy,1 Amr Hussein,2 Mostafa Mahmoud Eid, et al. “Cryptorchidism and Fertility.” Clin Med Insights Reprod Health. 2015; 9: 39–43. Clin Med Insights Reprod Health. 2015; 9: 39–43. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4689328/ |
| ↑16 | Thonneau, Patrick F., Candia, Peggy, Mieusset, Roger. “Cryptorchidism: Incidence, Risk Factors, and Potential Role of Environment; An Update.” Journal of Andrology Volume 24, Issue 2. March-April 2003. Pages 155–162. http://onlinelibrary.wiley.com/doi/10.1002/j.1939-4640.2003.tb02654.x/full |
| ↑17 | Brucker-Davis F, Pointis G, Chevallier D, Fenichel P. “Update on cryptorchidism: endocrine, environmental and therapeutic aspects.” J Endocrinol Invest. 2003;26(6):575–587. http://www.ncbi.nlm.nih.gov/pubmed/12952375 |
| ↑18 | Kaplowitz, P.B., S.E. Oberfield, and the Drug and Therapeutics and Executive Committees of the Lawson Wilkins Pediatric Endocrine Society. “Reexamination of the Age Limit for Defining When Puberty is Precocious in Girls in the United States: Implications for Evaluation and Treatment.” Pediatrics 104:4 (October 1999): 936–941. http://pediatrics.aappublications.org/content/104/4/936 |
| ↑19 | Herman-Giddens, M.E., E.J. Slora, R.C. Wasserman, et al. “Secondary Sexual Characteristics and Menses in Young Girls Seen in Office Practice: A Study from the Pediatric Research in Office Settings Network.” Pediatrics 99:4 (1997): 505–512. http://www.researchgate.net/publication/14123686_Secondary_Sexual_Characteristics_and_Menses_in_Young_Girls_Seen_in_Office_Practice_A_Study_from_the_Pediatric_Research_in_Office_Settings_Network |
| ↑20 | Colón I1, Caro D, Bourdony CJ, Rosario O. “Identification of phthalate esters in the serum of young Puerto Rican girls with premature breast development.” Environ Health Perspect. 2000 Sep;108(9):895-900. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2556932/pdf/ehp0108-000895.pdf |
| ↑21 | Aleksandra Fucic, Marija Gamulin,Zeljko Ferencic, et al. “Environmental exposure to xenoestrogens and oestrogen related cancers: reproductive system, breast, lung, kidney, pancreas, and brain.” Environ Health. 2012; 11(Suppl 1): S8. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3388472/ |
| ↑22 | vom Saal FS, Nagel SC, Benjamin L, et al. “The estrogenic endocrine disrupting chemical bisphenol A (BPA) and obesity”. Molecular and Cellular Endocrinology. Environment, Epigenetics and Reproduction 354 (1–2): 74–84. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306519/ |
| ↑23 | Gray LE Jr, Kelce WR, Monosson E, Ostby JS, Birnbaum LS. “Exposure to TCDD during development permanently alters reproductive function in male Long Evans rats and hamsters: reduced ejaculated and epididymal sperm numbers and sex accessory gland weights in offspring with normal androgenic status.” Toxicol Appl Pharmacol. 1995 Mar;131(1):108-18. http://www.ncbi.nlm.nih.gov/pubmed/7878665 |
| ↑24 | Kaylon L.Bruner-Tran, Kevin G.Osteen. “Developmental exposure to TCDD reduces fertility and negatively affects pregnancy outcomes across multiple generations?.” Reproductive Toxicology Volume 31, Issue 3, April 2011, Pages 344-350. http://www.sciencedirect.com/science/article/pii/S089062381000314X |
| ↑25 | Tyrone Hayes, Kelly Haston, Mable Tsui, et al. “Atrazine-Induced Hermaphroditism at 0.1 ppb in American Leopard Frogs” Environmental Health Perspectives. 111 (4): 568–75. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1241446/ |
| ↑26 | Hayes TB, Khoury V, Narayan A, et al. “Atrazine induces complete feminization and chemical castration in male African clawed frogs (Xenopus laevis).” Proc Natl Acad Sci U S A. 2010 Mar 9;107(10):4612-7. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2842049/ |
| ↑27 | University of Illinois College of Agricultural, Consumer and Environmental Sciences. “Atrazine is the main weapon against weeds in sweet corn, with few alternatives.” ScienceDaily. 5 May 2010. www.sciencedaily.com/releases/2010/05/100505102609.htm |
| ↑28 | Yucra, Sandra, Gasco, Manuel, Rubio, Julio. et al. “Semen quality in Peruvian pesticide applicators: association between urinary organophosphate metabolites and semen parameters.” Environmental Health 2008 7:59. http://ehjournal.biomedcentral.com/articles/10.1186/1476-069X-7-59 |
| ↑29 | Vested A, Ramlau-Hansen CH, Olsen SF, et al. “Associations of in utero exposure to perfluorinated alkyl acids with human semen quality and reproductive hormones in adult men.” Environ Health Perspect. 2013 Apr;121(4):453-8. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3620740/ |
| ↑30 | Fei C, McLaughlin JK, Lipworth L, Olsen J. “Maternal levels of perfluorinated chemicals and subfecundity.” Hum Reprod. 2009 May;24(5):1200-5. http://www.ncbi.nlm.nih.gov/pubmed/19176540 |
| ↑31 | Nicola Cherry, Harry Moore, Roseanne McNamee,et al. “Occupation and male infertility: glycol ethers and other exposures”. Occup. Environ. Med. 65 (10): 708–714. http://www.ncbi.nlm.nih.gov/pubmed/18417551 |
| ↑32 | Welch LS, Schrader SM, Turner TW, Cullen MR. “Effects of exposure to ethylene glycol ethers on shipyard painters: II. Male reproduction.” Am J Ind Med. 1988;14(5):509-26. http://www.ncbi.nlm.nih.gov/pubmed/3228067 |
| ↑33 | Nagano K, Nakayama E, Koyano M, et al. “Testicular atrophy of mice induced by ethylene glycol mono alkyl ethers (author’s transl).” Sangyo Igaku. 1979 Jan;21(1):29-35. http://www.ncbi.nlm.nih.gov/pubmed/470211 |


 Over the last 40 years, sperm counts have declined 59.3%–and are continuing to decline even as you read this
Over the last 40 years, sperm counts have declined 59.3%–and are continuing to decline even as you read this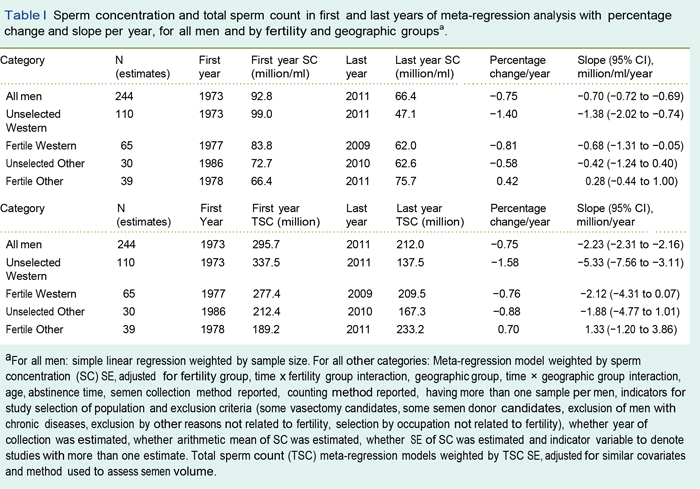










Hello Jon, thank you for the
Hello Jon, thank you for the article. you must have missed GMO and Glyphosate in your article. these seem to make a big difference in animal studies and on farms with animals. even how happy the animals are. maybe you could comment? maybe even mention the shikimate pathway, thank you
I eat lots of Brussel Sprouts
I eat lots of Brussel Sprouts, take a supplement of I3C, and Selenium to boost detox.
Also use standard carbon water filter but doesn’t seem to remove enough of the fluoride so I bubble jugs of the filtered water with Ozone for about 30 secs, and use a carbon filter on the shower-head.
The popular musician John Denver and his wife failed for yrs to have a baby, saw specialist all over the country and finally found out that his problem was Selenium deficiency.
I think you were quite remiss
I think you were quite remiss for not mentioning unfermented Soy.
Huh? He did, “To be sure,
Huh? He did, “To be sure, the phytoestrogens in soy formula and soy milk consumed to excess are likely to play a role, but, once again, we find xenoestrogens as a common thread in yet another reproductive crisis.”