Medical peer-reviewed journals are not the be-all and end-all when it comes to identifying which treatments work, and which ones don’t. Learn how you have paid over $1.5 trillion dollars for treatments, drugs, and procedures – all flawed, and all promoted at one time in peer reviewed journals.
Once again, the news forces me to return to one of my favorite topics — the limitations of medical studies and peer reviewed journals. Let me be absolutely clear here. Unlike many in the alternative health community, I am not anti allopathic-medicine. As I frequently remind people, after an automobile accident, you want a medical doctor, not an herbalist. There are things medical doctors can do that no alternative healer can replace. However!!! That said, as much as they would like to believe the contrary, medical doctors and modern medicine are not perfect. They do not hold an “exclusive” when it comes to providing the best option for treating all illness and disease.
But more to the point, the peer reviewed journals of the medical community are not the be-all and end-all when it comes to identifying what works and what doesn’t when it comes to treatment. So what set me off today?
- First, we received several emails at the Foundation over the last month from people asking, “If alternative health is so good, where are the peer reviewed studies to back it up?” We get these all the time, but this month more than usual.
- Second, yet another story broke about an extremely popular medical treatment that calls into question the value of peer reviewed studies.

With that in mind, let’s take a look at that story
Spinal cement sham
Okay, I’m going to spend a bit of time talking about a couple of procedures that probably aren’t of much interest to you unless you’re older and suffering from osteoporosis. But this isn’t actually about the procedures; it’s about their history and what that means. And that will be of interest to everyone.
Vertebroplasty and kyphoplasty, an explanation
Percutaneous vertebroplasty and kyphoplasty were developed in the mid-1980s as treatment options for compression fractures of the vertebrae. Vertebroplasty is a medical procedure where bone cement is injected through the skin and into a fractured vertebra in order to stabilize it. The procedure is typically used for a spine fracture caused by osteoporosis. Kyphoplasty is a related procedure in which an inflatable bone tamp is used to create a cavity in the bone so as to reduce the required injection pressure of the bone cement. It requires the use of slightly bigger needles than vertebroplasty, and therefore there is typically slightly more post-procedural pain. In laymen’s terms, kyphoplasty and vertebroplasty use glue/cement to reinforce the spine — kyphoplasty being merely a more expensive procedural variation of vertebroplasty. For years it was reported that both procedures were typically very effective and reduced pain in almost 90% of patients. In fact, there were peer reviewed clinical studies that attested to their effectiveness, such as the one on vertebroplasty published in the American Journal of Medicine back in 2003, or the one on kyphoplasty published in Spine three years later.
Vertebroplasty and kyphoplasty, the cost
 With results promising a 90 percent effectiveness rate, who wouldn’t opt for these procedures? And hundreds of thousands have done just that — guided, of course, by their doctor’s advice and encouragement. In fact, a veritable industry has grown up around these procedures with clinics springing up everywhere specializing in the procedures. For example: Fort Lauderdale Pain Medicine
With results promising a 90 percent effectiveness rate, who wouldn’t opt for these procedures? And hundreds of thousands have done just that — guided, of course, by their doctor’s advice and encouragement. In fact, a veritable industry has grown up around these procedures with clinics springing up everywhere specializing in the procedures. For example: Fort Lauderdale Pain Medicine
- Mayo Clinic
- Marshfiled Clinic
- SpineUniverse
And to what result? As of January 31, 2008, over 393,000 patients and 460,000 fractures worldwide had been treated with balloon kyphoplasty (since 2000 when the procedure was commercialized) at an average cost of $14,000 per procedure. For those of you not able to do the math in your head, that works out to about $6.5 billion spent on kyphoplasties over an eight year period in the United States alone. As for vertebroplasties, unfortunately, statistics are not as readily available. Suffice it to say, it has been around longer than kyphoplasty and is the de facto standard of care and is routinely offered to patients who complain of refractory pain. But for the sake of argument, let’s be conservative and say that merely the same number of vertebroplasties have been performed as kyphoplasties. At a cost of approximately $2500 per procedure, that works out to slightly over $1 billion. Combined, that means we’ve spent, in the United States, some $7.5 billion dollars on these two procedures over the last eight years.
With most of that money running through Medicare, one can only hope that your tax dollars are being spent wisely.
Vertebroplasty and kyphoplasty, the revelation
Unfortunately, two new studies published in the New England Journal of Medicine on August 5th tell a different story. According to these studies, the treatment of spinal compression fractures using cement (regardless of procedure) works no better than sham therapy in patients with osteoporosis. Basically, the studies tell us that we’ve just spent $7.5 billion on placebos.
The new studies are considered to be the most rigorously designed trials ever to examine the effectiveness of the cement treatment for the treatment of spinal compression fractures, effectively trumping all previous studies.
- A Randomized Trial of Vertebroplasty for Painful Osteoporotic Vertebral Fractures
- A Randomized Trial of Vertebroplasty for Osteoporotic Spinal Fractures
Now it is true that the two lead researchers differed in their interpretation of the implications for clinical practice.
Rachelle Buchbinder, PhD, who led the team of researchers studying “vertebral fractures,” was blunt. She said, “Our trial found no benefit for this treatment, so it should not be used in clinical practice.”
David F. Kallmes, MD, of the Mayo Clinic, who led the second study, was squishier and said that more research is needed to determine if certain patients respond better to the cement injections than to other treatments. But even he had to acknowledge the results of the study, “I think it’s fair to say that vertebroplasty does not work in the way that we thought it does, but it does work. It’s just that the (sham) treatment worked just as well and we can’t say why.” Congratulations Dr. Kallmes, that is an amazing piece of spin doctoring. A less “spun” translation might read, “I think it’s fair to say that a sham is a sham, and if something works no better than a sham, then it too is a sham.” All I can say is that if someone from the alternative health community had made a similar statement in support of a supplement, Dr. Kallmes would have been all over them in a heartbeat.
But let’s get real for a moment. It’s not like these studies came as a surprise. For a number of years now, there have been suspicions that the benefits received from cementing the spine may have resulted from the placebo effect. And in fact, some research hinted years ago that vertebroplasties might even be harmful in the long run because when one vertebra is shored up, adjacent ones may be more likely to break. In any case, the latest studies have once again exposed the fallacy that all medicine is science based. In fact, it is often faith based. As Dr. Joshua A. Hirsch, director of interventional neuroradiology at Massachusetts General Hospital in Boston, so aptly put it when commenting on the latest studies, “I truly believe these procedures work.” Now that’s pure science at work.
In any case, now that the new studies have been released debunking, at least to a large degree, the efficacy of the two procedures, the vultures (lawyers) have begun to circle.
The tip of the placebo iceberg
There are some in the medical community that call these latest studies an aberration, that overall medicines and medical procedures are overwhelmingly validated — that although there are more unproven therapies than they would like to see, those therapies are a significant minority.
I beg to differ.
Although you may dispute the actual percentage of treatments that lack scientific validation, you cannot dispute the overwhelming scope of their impact. And it should be noted that many treatments now listed in the “valid” column may ultimately turn out to be somewhat less than they appear — such as vertebroplasty and kyphoplasty. This alone skews the numbers significantly. But more importantly, as I just said, is the scope of the treatments that have been proven invalid.
I’ve covered a number of examples over the years, so I don’t want to go over them again in great detail — just highlight the important points and total up the dollars wasted.
And with that in mind, let’s start our running tab with the $7.5+ billion spent on spine cementing in the last decade.
Statin drugs
 In January of 2008, I wrote about the results from a study sponsored by Merck and Schering-Plough that found that after several years on two types of cholesterol-lowering medications, patients reduced their cholesterol level, but they reaped no significant health benefit at all unless they already had heart disease. (Note: Merck delayed releasing the results for two years, and only when finally pressed to do so.)
In January of 2008, I wrote about the results from a study sponsored by Merck and Schering-Plough that found that after several years on two types of cholesterol-lowering medications, patients reduced their cholesterol level, but they reaped no significant health benefit at all unless they already had heart disease. (Note: Merck delayed releasing the results for two years, and only when finally pressed to do so.)
But that’s not the worst of it. Just a few months later in October, I reported on the results of a study that found that Vytorin may increase the risk of cancer by 50 percent. In fact, this study found that Vytorin increased the risk of cancer in all major areas of the body. In addition, it found that among those who developed cancer, those taking Vytorin had a much higher rate of death than those taking a placebo.
And the bad news on statins just keeps rolling in like the tide in the Bay of Fundy. In July, I talked about a study published in the Canadian Medical Association Journal that confirmed that statin drugs cause structural damage to muscles. Even worse, the study found that muscle damage can continue to progress even after patients stop taking the drugs.
And how much do we pay for these dazzling results? In the US alone, sales of statin drugs generated approximately $19.7 billion in 2005 alone, or about $120 billion when averaged out over the last decade.
Breast cancer link to HRT and mammograms
 In February of 2009, I reported on a study that confirmed that postmenopausal women who take hormone replacement pills (synthetic estrogen plus progestin) for more than five years nearly double their risk of getting breast cancer. It seems inconceivable that given the evidence, medical professionals still would argue in favor of prescribing these drugs — and, yet, as many as 20 million women still do take them. But then again, the medical establishment cheered as more than 60 million women in the US alone signed up for the treatment annually prior to 2002.
In February of 2009, I reported on a study that confirmed that postmenopausal women who take hormone replacement pills (synthetic estrogen plus progestin) for more than five years nearly double their risk of getting breast cancer. It seems inconceivable that given the evidence, medical professionals still would argue in favor of prescribing these drugs — and, yet, as many as 20 million women still do take them. But then again, the medical establishment cheered as more than 60 million women in the US alone signed up for the treatment annually prior to 2002.
At a cost of $70-180 per month for Pempro, that works out to an average of $90 billion a year in the heyday for HRT drugs before 2002. And even at current usage, we’re talking about $30 billion a year, or $300 billion over the last decade.
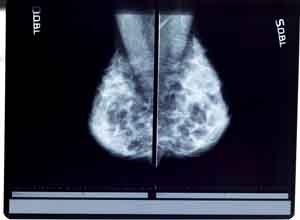
As for mammograms, a 2006 study found that fully one-third of all women interviewed were convinced that mammograms could invariably detect all cancers, no matter how small. But the truth is that 20 to 30 percent of the time, the mammogram can miss tumors. Plus, the rate of false positives, by some estimates, is as high as 90 percent or greater. And how many women are we talking about? Well, back in 2000, 70 percent of women in the US had regular mammograms, but that figure slipped to 66 percent by 2005, and the downward trend continues. But even if we accept an extremely low figure of 50 percent, you’re still looking at around 44 million mammograms a year in the US. And at an average cost of $100 per, that’s $4.4 billion a year, or $44 billion over a decade.
Angioplasty
And then there are angioplasties! In 2007, I reported on the study that found that angioplasties do not save lives or prevent heart attacks in non-emergency heart patients. In fact, the procedure only offers slight and temporary relief from chest pain, the main reason it is done. To quote from the study, “By five years, there was really no significant difference” in symptoms.
Unfortunately, studies now show that angioplasties aren’t very effective.
And how much money are we talking about with angioplasties. Every year in the US, doctors perform about 1.2 million angioplasties at an average cost of $40,000 apiece. That works out to $48 billion wasted every year in the US alone or $480 billion over the last decade –on just this one medical procedure!!!!
Antidepressants no better than placebos
 Antidepressant use in the US has nearly doubled since 1996, according to a study out of Columbia University and the University of Pennsylvania. As of now, antidepressants are the most commonly prescribed drugs in the US, at 118 million prescriptions a year. And how’s that working?
Antidepressant use in the US has nearly doubled since 1996, according to a study out of Columbia University and the University of Pennsylvania. As of now, antidepressants are the most commonly prescribed drugs in the US, at 118 million prescriptions a year. And how’s that working?
According to a report in The Wall Street Journal in January 2008, many studies have found that the best-selling antidepressants like Wyeth’s Effexor and Pfizer’s Zoloft may have little or even no effect on patients. Many of those studies, though submitted to the Food and Drug Administration, were left unpublished. Naturally, there was a response published in the New England Journal of Medicine arguing that doctors and patients may not have been able to see the full antidepressant picture. Well, that certainly explains away the results in a scientific manner!
So, how much do we pay for all this efficacy? According to some estimates, it works out to about $12 billion a year, or about $120 billion over ten years.
Conclusion
So add it all up, and what have you got? Actually, it totals up to close $1.5 trillion dollars spent every ten years on treatments that are out-and-out discredited, highly questionable, marginal, or in some cases, downright dangerous. And we’ve only touched the tip of the iceberg. We could have included:
- The anti-inflammatory, Vioxx, which was found to raise the risks of heart attacks and strokes — despite selling almost $2.5 billion a year.
- Then there’s Ritalin, which carries a black box warning issued by the FDA because of its highly addictive properties and potential for causing sudden death and serious cardiovascular damage. In fact, Ritalin’s side effect list includes an astonishing array of potential problems, ranging from the development of Tourette’s syndrome, to insomnia, psychosis, hypertension, hair loss, anemia, tachycardia and so on. Sales of Ritalin, Concerta, Adderall and other ADHD drugs increased to $3.1 billion in 2004, and is expected to reach $4.3 billion by 2012.
- And then there’s the report out of Stony Brook University in New York that confirmed that the cancer drug Avastin causes potentially lethal holes in the colon — a most distrubing side effect for a drug often prescribed for advanced colon cancer. Sales of Avastin run about $4.4 billion a year.
- And let’s not forget the huge, international study that found that children who received acetaminophen (Tylenol) even once in their first year of life had a 46% increased risk of developing asthma by age seven, as well as a 35 percent elevated risk of developing eczema and a 48 percent increased risk of having itchy eyes and runny noses. Sales of Tylenol are just under $1 billion a year — not bad for an over the counter drug.
- Etc., etc., etc. And on, and on, and on.
The bottom line is that I beg to differ with those who say that most medicine is based on good science and sound studies, and that the “occasional” stories you read are mere aberrations. At close to $1.5 trillion every decade, we’re not talking aberration — we’re talking terminal illness.
There are proven alternatives
 Which brings me to the final point: are there any alternatives to medications? And with that in mind, since we don’t have time to cover every drug and procedure discussed today, let’s just return to the issue that prompted this newsletter, spinal cementing. And, in fact, there are indeed alternatives to kyphoplasty and vertebroplasty. Surprisingly, many spinal fractures heal on their own and can be helped without surgery. This is especially true in younger adults.
Which brings me to the final point: are there any alternatives to medications? And with that in mind, since we don’t have time to cover every drug and procedure discussed today, let’s just return to the issue that prompted this newsletter, spinal cementing. And, in fact, there are indeed alternatives to kyphoplasty and vertebroplasty. Surprisingly, many spinal fractures heal on their own and can be helped without surgery. This is especially true in younger adults.
Then again, one of the most effective treatments and preventives is exercise — specifically, weight-bearing exercise. Weight-bearing exercise is exercise in which you force your body to support weight (your own included) while exercising. Studies have shown that weight bearing exercise can help slow down the rate of bone loss and osteoporosis, and therefore reduce fractures. How does it do this? First, weight-bearing exercise directly stimulates bone formation. Then, it strengthens muscles that in turn pull and tug on bones. This pulling action actually causes the bones to become denser and stronger. Weight-bearing activities at any age benefit bone health. Studies have shown that even people in their 90’s can increase bone mass with weight bearing exercise. One exceptionally useful form of weight bearing exercise is rebounding. The act of rebounding makes use of g-forces, just like astronauts training in a centrifuge. Rebounding can actually achieve momentary g-forces of 3.5, which means that the bones of a 150 lb person will momentarily have to bear 525 lbs of weight on each bounce. That’s a lot of weight bearing. Note: If you already have a weakened spine, you would need to build up to rebounding to avoid stressing the spine too much, too soon.
Certain nutritional aspects can also make a major difference in preventing bone loss. And no, I’m not talking about the current medical “wisdom,” which advises:
- Drink more milk.
- Take calcium supplements.
- Use HRT (hormone replacement therapy) to rebalance hormonal levels.
- Drink fluoridated water since fluoride builds bone mass.
- Use Fosamax, the latest wonder drug to prevent the destruction of bone.
If you go to a doctor and ask about osteoporosis, 99 percent of them will recommend some combination of the above. Unfortunately, this protocol just doesn’t work and actually contributes to osteoporosis. For more on preventing bone loss and understanding why the above steps don’t work, check out my newsletter on osteoporosis.
But that’s not the point of this newsletter. The point, as we have clearly seen, is that clinical studies in peer reviewed journals are decidedly limited. Yes, eventually, they may get things right, but often after years and years of waste and unnecessary injury and death. With well over a trillion dollars spent in just the last ten years on questionable treatments that at one time passed the peer review process, I think we can safely say the system is flawed.
Oh, and I almost forgot. There’s one other treatment for spinal fracture that studies have now shown to be virtually as effective as kyphoplasty and vertebroplasty — and it’s free. Or as Dr. Kallmes might say:
Take two placebos and call me in the morning.












"The bottom line is that I
“The bottom line is that I beg to differ with those who say that most medicine is based on good science and sound studies, and that the “occasional” stories you read are mere aberrations. At close to $1.5 trillion every decade, we’re not talking aberration — we’re talking terminal illness.”
You understand the meaning of most right? You’re degrading an entire field that is extremely large with new research coming in nearly everyday and using procedures that normally always work, by bringing up a few studies (which you said were fallacious) and concluding the medical field isn’t mostly scientific. Can you calculate all the money that went toward working treatments? I’m perfectly fine with improving the medical field where it needs it and prescribing less medicine in cases where they may not need it…but any readers who are a bit too credulous will jump to the conclusion that the medical field is bunk and just after money.
It IS bunk. They ARE after
It IS bunk. They ARE after money. And apparently they want to kill as many of us as possible in the process, as well. Read up on the American Dental Association and their campaigns for dental amalgams and water fluoridation, just to start. Add that to the ever-growing list of meds they push on us and the faulty dietary advice they give and it’s easy to see we are being poisoned to death. Just the amount of fluoride in foods and water is enough to ruin the average person’s health in the USA. If you’re also eating processed and GMO foods, God help you.