If you have high blood pressure, blood clots, or atherosclerosis, it’s imperative that you fully understand how that happened, the physiological consequences of any medical treatments, and any viable alternatives that might be available to you.
In today’s newsletter, we’re going to talk about the vascular system — your arteries and veins. Unlike our discussion of the heart, which required a great deal of anatomy, our discussion of anatomy today will be much simpler. As I’ve stated previously, my goal in this series is not to make you doctors, but to help you understand enough about your body’s systems and how they work so that you can communicate with your doctor and actively participate in your treatment. If you have high blood pressure, blood clots, or atherosclerosis, it’s imperative that you fully understand how that happened, the physiological consequences of any medical treatments, and any viable alternatives that might be available to you.
That’s what we will cover today.
Circulatory Systems
As we discussed previously, you have several distinct circulatory systems.
- The pulmonary system that carries deoxygenated blood away from the heart to the lungs, and then returns the refreshed oxygenated blood back to the heart.
- The systemic system that carries the oxygenated blood away from the heart out to every single cell in your body, and then returns the spent deoxygenated blood back to the heart so that it can be sent out through the pulmonary system.
- There is actually a third system, the portal system, which loops within certain organs or areas of the body that we will discuss in future newsletters.

The important thing to understand about these circulatory systems is that they are “closed looped.” Unless there is injury, no blood leaves them. As you will see, even the nourishment that every single cell in your body receives from your blood happens without that blood ever leaving the closed system. This becomes key when we talk about blood pressure.
The circulatory systems are comprised of:
- Arteries
- Arterioles
- Capillaries
- Veins
All told, these four components make up some 50,000 miles of passageways in the body. Let’s take a look at them in more detail.
Arterial system
Arteries, arterioles, and capillaries make up the arterial system. Arteries and arterioles have only one function—to move blood throughout the body. That’s all they do. They are channels, tubes, pipes if you will. As long as they are unclogged, flexible, and undamaged, they do their job. The primary difference between arteries and arterioles is one of size. Arterioles are just the smallest arteries you can see with the naked eye. Again, arteries and arterioles have only one function, to move blood. They do not feed any cells of the body—not even their own. That’s actually a fun little bit of trivia. The arteries of your body are not fed by the blood that flows through them. They require their own network of blood vessels called the vasa vasorum (literally, vessels of a vessel) that feed them — from the outside!
As I mentioned, I’m not going to get into naming all of the arteries in the body; but for the most part, arteries take their names from either the organs they supply (e.g.., the hepatic artery, which feeds the liver) or the areas through which they travel (e.g., the subclavian artery, which travels under the clavical—AKA, the collar bone).
Capillaries
Capillaries are quite different in function. They are not designed to shuttle blood. In fact, blood hardly flows through them at all as they are so small they allow only one blood cell at a time to pass through. Instead, the capillaries are the end point of the arterial system. It is in the capillaries that food and oxygen are exchanged with every cell in your body (except your cornea and the lens of your eye). Amazingly, of the 50,000 miles of circulation in the body, capillaries comprise over 49,000 miles.
Unlike the arteries, capillaries are invisible to the naked eye. They are smaller than a human hair—microscopic. And it is because they are so small and their walls are so thin, that capillaries serve as the exchange system for food and oxygen in the body. Keep in mind that every single cell in the body (except the cornea and lens) is near a capillary. That means that as blood passes through the ultra thin capillaries, it is easy for oxygen and tiny sugar and protein molecules (the end products of digestion) to “exchange” through the walls of the vessel and feed every single cell in the body.
Capillaries also serve as the connecting point between the arterial system and venous system that returns deoxygenated blood to the heart. The same exchange system that works to feed the cells of the body works in reverse. Cells pass their waste such as carbon dioxide back through the walls of the capillaries, where the blood cells recently relieved of their oxygen payload, can now pick up the CO2 waste from the cell and carry it back to the lungs for exchange with fresh oxygen.
Surprisingly, there’s more “space” inside the tiny capillaries than can be filled by your entire blood supply. If all your capillaries were “open” simultaneously, your blood pressure would drop precipitously, and you would die. What happens, though, is that your body intelligently shunts blood into different capillaries as needed. When functioning properly, this is a pressure regulating mechanism. The body can open more capillaries to lower pressure, and close off sections if needed to raise pressure.
Note: Our bodies retain the ability to sprout new capillaries throughout our entire lives.
Venous System
The venous system returns deoxygenated blood to the heart, and for the most part, it pretty much parallels the arterial system in all aspects—just in reverse. Whereas the arteries start out large (the aorta) and end small (the capillaries), the venous system starts small (the capillaries) and ends large (the vena cava). Veins tend to run right next to their corresponding arteries, and in fact have similar names. The subclavian vein, for example, runs in tandem with the subclavian artery under your collar bone. The primary exception is the vena cava, which is the aorta’s counterpart.
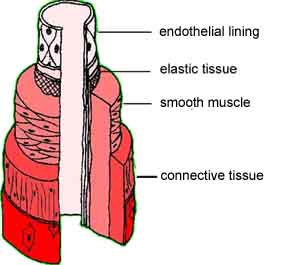
How arteries and veins are constructed
In this section, we start learning how problems occur. For it is their different construction (dictated by their different functions) that defines the nature of the things that can go wrong such as hardening of the arteries, high blood pressure, and blood clots.
Arteries
Arterial walls are composed of elastic tissue and smooth muscle. It is their elastic nature and the presence of substantial muscle tissue that allows them to expand and contract as the heart beats. This allows them to even out the increase in pressure caused by each beat. This is one of the primary reasons why hardening of the arteries (atherosclerosis) increases blood pressure. If you pump more fluid through the same sized tube, pressure must increase. On the other hand, if the tube is flexible and can widen, the increase is less. (We will talk more about this later.)
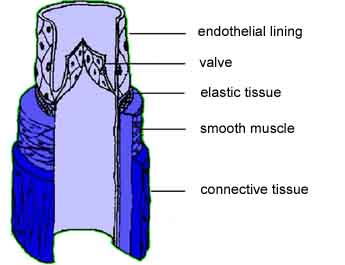
Veins
Veins are thinner walled than arteries and have less elastic tissue, and much, much less smooth muscle tissue. Instead, veins make use of valves and the muscle contraction of your body’s major skeletal muscles to squeeze blood along. This is the reason you’re asked to get up and walk around on a long plane flight—to prevent blood from pooling in your legs. As a side note, the lack of muscle in the walls of veins makes them more susceptible to bleeding when injured since there’s no muscle to clamp down.
Problems that can occur in arteries
There isn’t much mystery as to what the problem is—the build up of arterial plaque on the walls of the arteries and arterioles. There is, however, a great deal of mystery as to what causes it.
The basic problem is that arterial plaque (a combination of protein, calcium and cholesterol) starts building up on the walls of the arteries. This causes the arteries to both harden and narrow. So far so good! But what causes that buildup?
The cholesterol theory
The primary theory lays the blame on cholesterol—that as cholesterol levels climb in the blood, this causes plaque to form on the walls of the arteries. But this theory begins to collapse under even the most elementary scrutiny. As I mentioned in my newsletter, the Cholesterol Myth, one of my favorite questions to ask doctors is, “If cholesterol is the main culprit in heart disease, why don’t veins ever get narrowed and blocked?” And if you wanted to, you could throw capillaries into the equation too. Capillaries do not evidence the build up of arterial plaque. (They do, however, clog with amyloid plaque in the brain. But that’s a different problem that we’ll cover in a later newsletter.)
Think about this for a moment. If you have cholesterol circulating equally through the entire circulatory system, but it only causes plaque to build up in the arteries and arterioles, not the capillaries or veins, then how can cholesterol be the primary cause of the problem? If cholesterol caused plaque to form, wouldn’t it form everywhere? Since it only forms in the arteries, doesn’t the problem have to be something unique to those arteries?
The arterial wall theory
A more sophisticated version of the theory says that the build up of plaque is triggered by damage to the arterial wall—the endothelial lining. The lining consists of a thin layer of endothelial cells that performs two critical functions:
- It protects the “innards” of the artery from toxic substances in the blood.
- It helps regulate the expansion and contraction of the arteries by releasing a bio-chemical (cyclic GMP) into the cells of the smooth muscle in the arterial wall that change the tone or firmness of the artery.
In an attempt to repair damage to the endothelium, your body will “patch” the damage with plaque. This produces one of two conditions—two sides of the same coin really.
Artherosclerosis (hardening of the arteries)
Damage to the endothelial lining is “managed” by the smooth muscle cells surrounding the lining. Smooth muscle cells respond to endothelial injury by rapidly multiplying and producing a fibrin/calcium/cholesterol patch. These patches, called plaques occur just inside the lining and thicken the artery’s inner wall. Over time, given multiple injuries, the wall of the artery begins to harden and become dysfunctional, no longer expanding and contracting to regulate blood pressure —and steadily narrowing the passageway through which blood flows.
Arteriosclerosis (plaque build up)
Another way of describing this process is that your body creates plaque to “paste over” any damaged areas—like a scab over a cut. Over time, given repeated injury, these plaques intrude more and more on the inner passage of the artery steadily compromising the ability of the artery to expand and contract and for blood to flow freely.
But it gets worse
The damage to the arterial wall also triggers an immune response with white blood cells flooding the area. This leads to a chronic inflammatory response in the blood vessel. Continued inflammation causes even more damage, which accelerates the process.
All of this, of course, brings up the $64,000 question: “Since the entire theory hinges on damage to the endothelial lining, what actually causes the damage to the lining, and why doesn’t it happen to the lining of the veins?”
Once again, oxidized fats and LDL cholesterol are named as the key culprits. Other suspected culprits include:
- Free radicals.
- High blood pressure (yes, high blood pressure begets more high blood pressure).
- Diabetes.
- High homocysteine levels.
- High C-Reactive Protein levels.
- Low levels of vitamin C (similar to scurvy).
- Low levels of nitric oxide.
- Heavy metals.
- Aging.
Muscle matters
But once again, the question arises: “Are not all of these things present in the capillaries and veins too?” The answer, of course, is yes they are—which means there’s still a missing piece in the equation. The answer, according to the pH theory, lies not in what flows through the arteries and veins (which is identical), but in their construction (which is different). The key difference between arteries and veins is in the amount of muscle tissue surrounding the endothelial lining. In arteries and arterioles, the smooth muscle is extensive. In veins, it is minimal. And in capillaries, it is totally absent. Why does this matter?
It matters because when muscle tissue is used it produces lactic acid. If your body is healthy (in an alkaline state) and has ready access to an abundant source of oxygen rich blood, that lactic acid can clear quickly. But for those people who eat a high acid forming diet and are in an acidic state, the lactic acid cannot clear quickly. (Remember, blood vessels do not have direct access to the oxygen in the blood that flows through them. They are dependent on the vasa vasorum.) It is the lactic acid that provides the final trigger that causes damage to occur in arterial linings, but not so in veins. It is the presence of accumulated lactic acid in the smooth muscles surrounding arteries that ultimately causes plaques to form.
But even beyond lactic acid, there’s another area where muscle tissue matters: nitric oxide. The contraction of the muscles in the arterial walls is regulated by a signaling molecule that we referred to earlier called cyclic guanosine monophosphate (cyclic GMP) in the muscle cells. Cyclic GMP causes the arterial muscle to relax, in preparation for its next contraction. Cyclic GMP is triggered by nitric oxide, which is produced in the endothelial lining. The ability of the lining to manufacture enough nitric oxide to maintain artery dilation is one of its most crucial functions. As damage continues to build in the lining, it blocks nitric oxide-induced dilation, thus stiffening the arteries.
High Blood Pressure
If the arterial blockages happen in your coronary arteries, the result, as we’ve discussed previously, is coronary heart disease and a heart attack. If it happens in the carotid arteries leading to the brain, it can cause a stroke.
In most cases, however, the damage happens systemically, throughout your arterial system, and the result is high blood pressure. As a quick review, blood pressure is a measurement of the two pressures in your circulatory system as your heart beats. The increased pressure produced in your circulatory system by the contraction of the left ventricle is referred to as systolic pressure. The reduced pressure during relaxation is called diastolic pressure. These are the two numbers your doctor gives you when reading your blood pressure (e.g., 120 over 70). Both low and high blood pressure are dangerous, but low blood pressure is usually easier to manage. High blood pressure, on the other hand, tends to be more intractable and harder to manage—and therefore more dangerous.
Your body has many mechanisms for controlling blood pressure.
- It can change the amount of blood the heart pumps.
- It can change the diameter of arteries, and the volume of blood in the bloodstream.
- To increase blood pressure, it can pump more blood by pumping more forcefully or more rapidly.
- It can also increase pressure by narrowing arteries (particularly the arterioles), forcing the blood from each heartbeat through a narrower space than normal.
- It can seal off capillaries forcing the blood into a smaller space, thereby increasing pressure.
- The body can add fluid to the bloodstream (regulated by the kidneys) to increase blood volume and thus increase blood pressure.
- And it can remove fluid from the blood (also regulated by the kidneys), thereby decreasing pressure.
All of these things happen automatically, regulated by a healthy body, without your even thinking about it. In addition, blood-pressure measurements can vary throughout the day, affected by everything from:
- Food.
- Alcohol.
- Caffeine.
- Smoking.
- Stress.
- Climate.
- And the time of day.
- Blood pressure changes that occur naturally during the day are the result of the body’s internal (circadian) rhythms. In most people, blood pressure rises rapidly in the early morning hours, in anticipation of rising and beginning the day. This is not the result of the physical act of rising but is a preset system that automatically increases a person’s blood pressure at that time. Likewise, pressure normally starts dropping early in the evening in anticipation of going to sleep.
All of these things mentioned so far, have nothing to do with clinical hypertension unless they result in secondary damage such as can be caused by smoking and alcohol or sustained stress. Clinical hypertension is a chronic and dangerous condition caused by:
- Constricted arteries.
- Hardened arteries.
- Malfunctioning kidneys (which we’ll talk about in a subsequent newsletter).
If left untreated, chronic hypertension can cause:
- Damage to the heart muscle because of the extra load it puts on the heart.
- Strokes.
- Kidney damage—which leads to more hypertension, which leads to more kidney damage, etc.
And ultimately, it kills you.
Problems that can occur in veins
As we’ve already discussed, veins do not have a substantial amount of muscle tissue to contract and squeeze blood along. That means that without physical activity to cause the skeletal muscles to squeeze the veins:
- Blood has a tendency to pool and stop flowing in veins—particularly in the legs where gravity works against you.
- Blood that isn’t flowing tends to clot.
- Clots tend to propagate more clotting around the original clot.
- Cumulatively, this can form very large clots.
Large clots that stay in place and block the flow of blood cause phlebitis.

If the clot breaks free and starts traveling through the circulatory system, it’s called a thrombus. At whatever point it lodges in a blood vessel and blocks it, it’s called an embolism. If you think back to our discussion of the venous system, you’ll remember that veins get steadily bigger as blood moves back to the heart. That means that clots that break free in the legs are unlikely to be stopped anywhere on their way back to the heart. The first place they are likely to lodge is when the right ventricle of the heart pumps them out into the pulmonary circulatory system on the way to the lungs. If the clot is fairly small, it will lodge in the lung itself and block the flow of blood to a section of the lung, killing it. This is called a pulmonary embolism. Larger clots can actually lodge in the pulmonary artery feeding an entire lung…killing the lung just like that. Or the clot can lodge at the juncture where the pulmonary artery divides between the two lungs, which will kill both lungs simultaneously…in an instant.
DVT, or deep vein thrombosis, is the term now commonly associated with clots that form as the result of prolonged sitting on an airplane. They tend to break free the next time you start moving again with any vigor. This can be several days or weeks after the plane flight itself, which means many people never connect the two events.
There is one other notable place that clots tend to form. As a result of low blood flow or damaged valves, clots can form in the left atrium of the heart. If the clot forms there, it’s already past the pulmonary circulatory system so it can’t affect the lungs. Unfortunately, the next stop for the clot is out into the systemic circulatory system, where it has a good chance of being pushed up into the brain causing a stroke.
What doctors do about these problems
Medical treatments for vascular problems never address the actual causes, but seek instead to force test results back into line. What is your doctor likely to offer?
Clogged arteries
Modern medicine really only has two approaches.
- Surgically repair the damaged area (bypasses and angioplasties).
- Use drugs to improve the flow of blood through the damaged area and minimize the production of cholesterol, which serves as one of the triggers.
Neither of these approaches, of course, actually deals with the real problem.
High blood pressure
When it comes to high blood pressure, doctors rely almost exclusively on pharmaceutical drugs. The four major classes of drugs are:
- Diuretics, which reduce pressure by making you pee out water from your body. Reduce the volume of fluid in your blood, and you reduce the pressure. Unfortunately, side effects can include dizziness, weakness, an increased risk of strokes, and impotence. (Not to worry, there are medications to alleviate the side effects.)
- Calcium channel blockers, which work to relax and widen the arteries—thus reducing blood pressure. Then again, a major side effect of channel blockers is a 60% increased risk of heart attack.
- Beta blockers, which work by weakening the heart so it won’t pump as strongly, thereby reducing blood pressure. One of the major problems with beta blockers, though, is the increased risk of congestive heart failure.
- ACE inhibitors (the new drugs of choice), which like the calcium channel blockers, also work to relax and widen the arteries. Unfortunately, ACE inhibitors can produce severe allergic reactions, can be deadly to fetuses and children who are breastfeeding, and can cause severe kidney damage.
Again, none of these drugs deals with the actual cause of the high blood pressure. They are merely an attempt to force test numbers into line and prevent people from immediately dying.
Blood clots and DVT
If doctors are worried about clots (such as after bypass surgery), they put patients on blood thinners. The standard is Coumadin (warfarin). Aside from the usual jokes that Coumadin is essentially rat poison (which it is), it has serious side effects. It can cause severe internal bleeding that can be life-threatening and even cause death. You can always tell a person on warfarin by the extensive bruising all over their body since even the slightest bump or touch is enough to cause internal bleeding. It’s a bit like using dynamite to open a locked door. It can do the job, but you need to be oh so careful or you’ll blow up the building at the same time. There are better choices.
Note: Some people might think aspirin is a good alternative. It’s not. While aspirin may be beneficial at keeping blood flowing through arteries, studies indicate it has no effect on preventing clots from forming in veins.
What are the options?
As it turns out, for most major heart problems, you have a world of alternatives—certainly safer and often far more effective than their medical counterparts.
Clogged arteries
- Studies have shown that dietary changes alone can unplug arteries.
- Proteolytic enzymes, particularly formulas that contain either nattokinase or lumbrokinase, can break down the proteins that hold plaque together stuck to arterial walls—effectively dissolving it.
- Proteolytic enzymes can also help dissolve scarring of the endothelial lining.
- And proteolytic formulas that contain seaprose-s or serrapeptase can help reduce arterial inflammation that both constricts arteries in real time and contributes to future long term damage.
- Sufficient Omega-3 fatty acids in the diet also help reduce arterial inflammation and dramatically reduce the circulating levels of damaging NEFAs.
- Antioxidants such as SOD, pomegranate, grape seed extract (AKA OPCs), and pycnogenol help heal the endothelial lining, thereby preventing future plaque and helping to heal current plaque.
- Methylating supplements such as B6, folic acid, B12, TMG, and SAMe help reduce homocysteine levels, thereby reducing damage to the endothelial lining.
- L-arginine and noni extract assist the smooth muscle in arterial walls in obtaining sufficient nitric oxide to function properly.
- Regular heavy metal detoxing can reduce a major cause of irritation to the endothelial lining and a primary instigator of plaque formation.
- And raising body pH through proper diet and the use of supplements such as coral calcium reduces lactic acid levels in the arterial smooth muscle, thereby minimizing damage to arterial linings.
As you can see, there is a world of choices you can make that can dramatically change your vascular outcomes. Virtually all of them are covered if you’re following the Baseline of Health® Program.
High blood pressure
Pretty much everything you do to reduce clogging of the arteries will, by definition, help to reduce blood pressure. In addition, though, you can also consider:
- Lose weight. Simple laws of physics apply here. As we’ve already discussed, your blood vessels have to service every single cell in your body. The more body mass you have, the more pressure you need to force blood through the system. Lose weight; less pressure required.
- If you smoke, stop. Smoking constricts blood vessels and raises pressure.
- If you’re stressed, try meditation or biofeedback. As part of your body’s “flight and fight” mechanisms, stress increases heart rate and blood pressure to help respond to the short term stress of an attack from a saber toothed tiger. Twenty-four/seven stress was not designed into the system. Prolonged stress definitely impacts blood pressure levels. Even if you have clogged arteries, reducing stress levels can still help drop your blood pressure levels significantly.
- Herbs such as passionflower, apocynum venetum, hawthorne, and stevia (yes stevia) have all been shown in clinical studies to help lower blood pressure.
Blood clots and DVT
Proteolytic enzymes, particularly formulas that contain either nattokinase or lumbrokinase are just as effective at preventing clots, with wide ranging dosage tolerances. In other words, good proteolytic formulas work with minimal chance of side effects. In fact, a good systemic proteolytic enzyme formula that also contains enzymes such as endonase, seaprose-s, or serrapeptase can have multiple beneficial effects for the circulatory system in addition to reducing clotting. Such formulas can play a major role in reducing inflammation and scarring in the cardiovascular system and enhance cardio perfomance in athletes.
Conclusion
When it comes to most forms of heart disease associated with the arteries and veins, you have a world of alternatives—certainly safer and often far more effective than their medical counterparts. It’s also worth noting again that if you are following the Baseline of Health® Program, then you’re already doing most of them.
Which brings us to the final part of our series on the anatomy, physiology, and diseases of the cardiovascular system—your blood. In the next issue will take on this most complex of subjects.
Read more about Heart Disease Prevention











Proteolytic enzymes. Given
Proteolytic enzymes. Given their propensity to break down scar tissue are they not recommended for people who have had an aneurysm coiled?
William
do any of these herbs or
do any of these herbs or enzymes react with antirejection medication for a kidney transplant?
My husband has been taking
My husband has been taking warfarin for more than 20 yrs. That must not be good! I cannot believe that after 60 yrs. of the invention of warfarin, there is no natural substitute. There are may natural foods out there with anti-couagulant properties but there’s no way to taking an exact dose. Is there anything you know about?
Sonia:
Sonia:
There certainly are natural compounds that thin the blood, such as the enzymes mentioned above, fish oil, and vitamin E I believe, but though they thin blood, they are not studied or ” proven'” so you are on your own. There are now in home testing unites for blood thinning. If you have the courage you could experiment at home. What should drive you to consider abandoning warrafin is the fact that it poisons vitamins K1 and K2. K2 is responsible for proper calcium deposition, and without it , calcium is lost from bone and teeth and deposited in soft tissue such as arteries, heart valves, and joints. The good news is that this process is restorable. See the recent book Vitamin K2 and the Calcium Paradox: How a Little-Known Vitamin Could Save Your Life by Kate Rheaume-Bleue
At least find a doctor or natural path that can assist in
supplementing with K2 if you continue with coudamin. Try searching for a member of the American College for Advancement in Med
John Wagoner
I know some supplements
I know some supplements contained proteolytic enzymes but I doubt to use it as blood thinner. can we consume these kind of enzyme along with blood thinner such as clopidogrel?
You do not want to take
You do not want to take systemic proteolytic enzymes without food if you’re on blood thinners. You can, however, probably take digestive enzymes that contain proteolytic enzymes with food. Check with your doctor.
What is your view on the
What is your view on the theory of stress hormones contributing to scarring of the arterial walls leading to plaque buildup.
There is certainly some
There is certainly some research that indicates such a connection. http://www.ncbi.nlm.nih.gov/pubmed/19453564
Would proteolytic enzymes
Would proteolytic enzymes dissolve scar tissue inside the coronary arteries that formed from healing of a spontaneous coronary artery dissection?
Although proteolytic enzymes,
Although proteolytic enzymes, given enough time, can dissolve some forms of internal scar tissue, there are no studies that demonstrate its effect for this particular condition. That doesn’t mean that they wouldn’t help—only that there is no track record.
My wife has suffered from
My wife has suffered from very high blood pressure for many years. She retired from paid work about three years ago but always kept working in spite of her problem. Things got worse after her retirement and she grew weak and looking for an operation was told this was not possible . However we discovered Jon’s proteolitic enzymes and her strength improved and her aorta valve was replaced successfully. Though she has made big improvements since the operation and takes only proteolitic enzymes + natural remedies she recently had extra problems with restless legs syndrome–and her blood pressure of even 200 by 110 sometimes remains. She eats very carefully only a vegetarian diet but eats fish. Yet we wonder if, somehow, her arteries are partially blocked with plaque and she has begun drinking ionised water to help clear her pulmonary and systemic circulations and improve her blood quality. Hopefully this will lower her blood pressures in this very stubborn case of hypertonia?