In this issue, we examine the composition of blood and how that determines its functionality.
In the last issue of the newsletter, we discussed the three primary functions of blood in the human body: transportation, protection, and balance. In this issue, we’re going to examine blood components and how they determine blood functionality. Why is this important? Two reasons:
- When your doctor runs tests on your blood, he/she is primarily looking at the individual components—like hematocrit, albumin, platelet, and white cell counts. Knowing what your doctor is talking about and what the levels mean will empower you to be an active participate in any treatment. (In the next newsletter we will cover these tests in detail.)
- Knowing what the pieces are and what affects them will give you access to a world of alternatives that your doctor is unlikely to inform you about—or to be inforfmed about themselves, for that matter.
So let’s begin. In simple terms, the composition of blood is 55% plasma and 45% formed elements (red cells, white cells, and platelets). Ah! But in that simplicity is a world of complexity. (Note: don’t get lost in the details. Just follow the basic principles. In the next newsletter, we’ll refocus on the important parts.) For now, let’s just explore .
Plasma
Plasma is the clear yellow liquid that serves as the transportation agent in blood. It is mostly water, some 91.5%, in fact. The rest is 7% protein and 1.5% other solutes.
Proteins in blood plasma
The proteins in blood function primarily as clotting agents and antibodies. Abnormal levels are indicitive of everything from autominnune disorders to cancer to heart disease. The key ones are:
- Albumins 50-60%: Serum albumin is the most abundant blood plasma protein and is produced in the liver. The human version is called human serum albumin, and plays a key role in regulating blood volume by maintaining the osmotic pressure of the blood compartment. It also works as a binding agent for bilirubin, free fatty acids, testosterone, calcium and some drugs. Low albumin may be caused by liver disease, kidney disease, burns, malnutrition, late pregnancy, genetic variations, and even bad posture. High albumin is often caused by dehydration.
- Globulins 38%: This is a generic term to describe several different families of proteins which have larger molecules than albumin and are less soluble in pure water. They include:
- Alpha globulins, which control and inhibit certain blood enzyme activity. Malignancy and acute inflammation can increase the levels of alpha globulins in the blood. A low level is often indicative of liver disease.
- Beta globulins, including:
- Plasminogen, which converts to plasmin, when needed, to help break down blood clots.
- Angiostatin, which inhibits the formation of new blood vessels and may play a role in cancer therapy.
- Sex hormone binding globulin, which like albumin plays a role in the transportation of sex hormones through the bloodstream.
- Gamma globulins, which function as antibodies and play a major role in immune function. Low gamma globulin levels are seen in people who donate blood too often or have immune system problems.
- Fibrinogen 7%: Fibrinogen is converted, as needed, into fibrin. Whenever there is trauma to the arterial system, fibrin forms itself into a mesh at the site of the injury to capture blood platelets and form a temporary plug over the wound site. Fibrinogen levels are a reflection of clotting ability and activity in the body. Chronically low levels may be related to decreased production due to an inherited condition or to an acquired condition such as end-stage liver disease.
- Other proteins, such as C-reactive protein, comprise the rest of the proteins—about 1.5%. High levels are a marker for systemic inflammation and are a predictor of heart disease.
Other solutes in blood plasma
The non-proteins dissolved in blood plasma make up about 1.5% of the plasma and include things such as:
- Electrolytes: These are the minerals dissolved in your blood (and other body fluids) that contain free ions and carry an electric charge. It is important that the balance of electrolytes in your body be maintained, because they affect the amount of water in your body, blood pH, muscle action, and a host of other important processes including the beating of your heart. Electrolytes exist in the blood as acids, bases, and salts such as sodium, calcium, potassium, chlorine, magnesium, and bicarbonate. You lose electrolytes when you sweat, and they must be replenished or your body will lose the ability to perform effectively, or even die.
- Nutrients.
- Gasses (oxygen, carbon dioxide, and carbon monoxide if you’re unlucky).
- Regulatory substances (such as insulin to regulate blood sugar and various immune regulating molecules).
- Vitamins.
- Waste such as urea.
Formed elements
As we said earlier, plasma comprises 55% of blood. The other 45% is made up of the non-soluble “formed elements.” Specifically, we’re talking about:
- Platelets
- White blood cells (leukocytes)
- Red blood cells (erythrocytes)
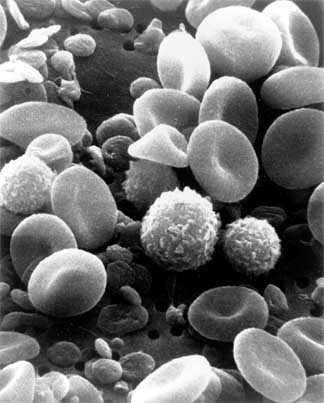
This is a scanning electron microscope image from normal circulating human blood.
One can see red blood cells, several white blood cells including lymphocytes,
a monocyte, a neutrophil, and many small disc-shaped platelets.
Platelets
Although platelets are often classed as blood cells, they are actually fragments of large bone marrow cells called megakaryocytes. As fragments, they are generally disc-like, but irregular in shape. In effect, they look like broken plates—thus their name. In normal blood there will be between 250,000—400,000 per ml of blood. The role of platelets is to assist in blood clotting. During normal blood clotting, the platelets clump together, or aggregate at the site of an injury.
Essentially, they are part of the body’s initial blood clotting response. When there is external or internal trauma, or there is damage to endothelia cells (such as those that line the inside of the blood vessels) or collagen has been exposed in internal tissue, the body rushes platelets to the site of the injury, where they clump together to form the initial plug to seal up the wound.
This all sounds simple enough, but the control mechanisms are, in fact, remarkably elegant.
When collagen is damaged it releases ADP (Adenosine diphosphate). ADP is what is known as an agonist, a substance that binds to a specific receptor and triggers a response in a specific cell. By itself, ADP is a strong agonist, but its effect is greatly amplified in the presence of adequate levels of serotonin. (If levels of either ADP or serotonin are low, the clotting effect is significantly lessened.) ADP works by triggering platelets to change shape, release granule contents, and clump together. Upon exposure to activating agonists, such as ADP and serotonin, platelets break down arachidonic acid in the blood to form thromboxane A2, which plays a major role in the activation and recruitment of more platelets to add to the plug. ADP also causes adhesion of platelets to atherosclerotic plaques and to the walls of the injured arteries.
But we’re not done yet.
Once the leak is plugged and the “emergency” is over, the blood then works to form a more permanent clot. In fact, it is the formation of the original clot that triggers the humoral coagulation system, leading to the creation of a more permanent clot. Or to put it another way: clotting begets clotting. Even as platelets plug the injury site (a process called primary hemostasis), secondary hemostasis is already kicking in. In secondary homeostasis, proteins in the blood, called coagulation factors (fibrinogen, prothrombin, etc.), respond in a complex cascade to form fibrin strands which strengthen the platelet plug. The coagulation cascade of secondary hemostasis is very complex and actually follows two separate pathways. It is beyond the scope of this newsletter, but for those who are interested in learning more, check it out here.
The key things to remember about the clotting process are:
- It is finely tuned
- It is self regulating. Certain proteins initiate the process. Other proteins reinforce the process. And still other proteins (such as plasminogen) keep it from running out of control—in other words, stop the clot from spreading throughout your entire body.
- Remember, clotting begets clotting. Thus the need for bio-chemicals in the blood such as plasminogen to moderate the process.
It should be noted that hemophiliacs have platelets. What they’re missing is one or more of the “follow up factors” ( usually Factor VIII) that are necessary to produce more stable clots. Whereas, severe hemophilia was at one time pretty much an eventual death sentence, not so much any more. Doctors simply replace the missing clotting factors with clotting factors extracted from human blood donated to blood banks. (Incidentally, obtaining clotting factors is not a problem since they are removed from all blood used for transfusions so that the blood does not clot prematurely.) There are no natural treatments that are as effective. This is one place where doctors definitely trump natural healers.
Leukocytes – white blood cells
All blood cells, both red and white, begin as stem cells in your bone marrow. These undifferentiated cells begin to assume individual characteristics and become either red cells (the oxygen carriers) or white cells (the cells of the immune system). Incidentally, the literal translation of the word leukocyte is “white cell.” White cells make up about 1% of your blood and number about 5-10 thousand per ml.
Since white cells really are the cornerstone of your immune system, we’ll save a detailed discussion of their function for a later newsletter when we explore that system in detail. For now, we’ll just take a quick look. Further differentiation divides the leukocytes into four main types of cells:
- Lymphocytes
- T-cells – distinguish between normal healthy cells and invaders, including mutated rogue cells.
- B-cells – make one specific antibody to defend against one specific invader.
- NK-cells – attack a whole range of microbes and tumor cells.
- Phagocytes
- Neutrophils – main bacteria fighters.
- Monocytes – along with the neutrophil, the major microbe-eating and killing cell in the blood. When monocytes leave the blood and enter the tissue they are converted to macrophages.
- Macrophages – attack foreign invaders and eat up worn out cells and other waste in the body.
- Granulocytes
- Eosiniphils deal with allergies.
- Basophils are allergy processing.
- Mast cells—mount a response to parasite and bacterial infection.
- Dendritic cells wrap up antigens and spent lymphocytes and carry them to the lymph nodes for removal from the body.
Note: in leukemia, the number of white cells climbs from 5-10 thousand per ml to as much as 100-400 thousand malignant cells per ml.
Erythrocytes – red blood cells
When people think of blood, it’s really the erythrocytes they’re thinking of. It’s the erythrocytes that give blood its red color. In fact, the name erythrocyte means “red cell.” The erythrocytes also perform the function most people equate with blood—carrying oxygen to the cells and carbon dioxide out of the body. Red blood cells make up about 45% of blood’s total volume and number about 4.8 – 5.4 million cells per ml. This volume is expressed by doctors as the “hematocrit level.” A level of 45% is obviously cool; less than that is anemic —with levels below 30% considered severely anemic. Another term that’s important when talking about red blood cells is “hemoglobin.” Hemoglobin is the iron-based metalloprotein molecule inside the red blood cells that actually carries the oxygen and carbon dioxide. The name hemoglobin comes from the joining of the two words heme and globin, reflecting the fact that hemoglobin is made from a globular protein with an embedded heme group. Each heme group, or cofactor, contains an iron atom, which is responsible for the binding of oxygen. There are approximately some 250-300 million hemoglobin molecules in each blood cell, and they comprise about 1/3 the total hematocrit volume—weighing in at 13-14 grams.
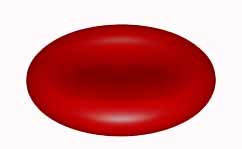
The design of a healthy red blood cell is important. It’s very, very small, about 6-8 microns (.00025 inches) in diameter, and its shape is that of a bi-concave disc. Both its size and shape are optimized for carrying and easily exchanging gases. Red blood cells can also easily fold to facilitate their movement through tight spaces in tiny capillaries. One other interesting fact about erythrocytes is that they have no nuclei. They don’t need it since they have only one function: to transport and exchange gases. In fact, fact red blood cells are designed to have a high affinity for oxygen and a moderate affinity for carbon dioxide. This affinity is further augmented (and regulated) by body and blood pH. pH is geared for the release of carbon dioxide and the uptake of oxygen in the lungs, but a slight adjustment in pH regears the blood cells for release of oxygen and the uptake of carbon dioxide at the tissue level. It’s brilliant!
Note: in the last newsletter we talked about hemoglobin’s preference for carbon monoxide, which can lead to carbon monoxide poisoning. In fact, hemoglobin prefers carbon monoxide over oxygen by a factor of 200 times!! It refuses to let go of the carbon monoxide, keeping it in circulation for quite some time. You literally have to force oxygen into the blood to dislodge it.
It should be noted that red blood cells have a very short life cycle of about 120 days. That means that every four months you replace every single red blood cell in your body. This means that the production rate of red blood cells is phenomenal—around 2.5 million new cells per second, or a mind boggling 200 billion new cells each and every day of your life. To accomplish this feat, your body needs several key nutrients…all present 24/7:
- Amino acids (proteins) for producing the globular protein part of the hemoglobin.
- Iron for the production of the heme non-protein cofactor portion of the hemoglobin.
- Vitamins B12, B6, and folic acid.
- Nickel and cobalt as trace minerals.
- Erythropoietin (EPO), a hormone, is produced in the kidneys and plays a key role in regulating production of red blood cells. It has a history of usage as a blood dopingagent in endurance sports such as bicycle racing, triathlons and marathon running. Production and release of EPO is governed by:
- The need to keep the normal oxygen carrying capacity of the blood at a steady state based on the normal turnover of erythrocytes.
- The oxygen content of tissues. Low oxygen levels in body tissue leads to increased production or EPO.
The making of blood cells—both white and red
Again, all blood cells, both red and white, begin as stem cells in your bone marrow. As stem cells mature, they undergo changes in their gene expression. This limits the cell types they can become and moves them closer to a specific cell type. Each successive change moves the cell closer to its final choice of cell type and further limits its potential cell type until it is fully differentiated. This is really an incredibly cool subject, and we could spend days on it—not very practical at this time. So let me focus on some of the highlights, to give you an idea of how brilliantly it all works.
Human bone marrow stem cell
Under the influence of various bio-chemicals in the body, the human bone marrow stem cell becomes one of two different cells:
- Common lymphoid progenitor
- Common myeloid progenitor
Again, under the influence of various bio-chemicals, these two types of cells are transformed. After undergoing several intermediary stages, the common lymphoid progenitor evolves into T-cells, B-cells, NK-cells, and dendritic cells. The common myeloid progenitor follows a more complex evolution. It first evolves into four entirely different types of cells:
- Megakaryoblasts
- Mast cells
- Myoblasts
- Proerythroblasts (aka rubriblasts)
These four types of cells then follow straight line evolution through several intermediary stages as follows:
- Megakaryoblasts actually go through a couple of evolutions, and then literally break apart—into a multitude of pieces—thus forming platelets.
- Mast cells become mast cells after a single evolution from common myeloid progenitor cells so no further evolution is required.
- Myoblasts break into four separate pathways, which ultimately evolve into: basophils, nutrophils, eosinophils, and macrophages.
- Which leaves the proerythroblasts, which largely under the influence of EPO (the kidney hormone discussed above), go through five evolutions to ultimately become red blood cells.
The important thing to understand here is that this is an incredibly complex process that requires everything to be in place and proper balance to be maintained in order to function correctly. With this in mind, it’s not hard to see why you can’t build the same blood cells out of pepperoni, pizza, beer, and Ding Dongs that you can out of real food that’s packed with real nutrients, vitamins, minerals, and trace minerals. If you’re light just one component at a critical juncture in the process, the resultant cells will be compromised. If you have some extra hormone-like chemical (from the 100,000 plus that have been released into the environment over the last hundred years) intervene in the process, you can send the cell evolution off into uncharted waters.
Proper nutrition matters. Toxicity matters. And yes, genetics matters.
Sickle cell anemia
Sickle cell anemia occurs when a person inherits two abnormal genes (one from each parent) that cause their red blood cells to change shape. Instead of being flexible and disc-shaped as described above, sickle cells are more stiff and curved—in the shape of a sickle, which is where the disease gets its name. Sickle cells are also stickier than normal, which makes them tend to stick together causing the blood cells to clump and clog blood vessels. Also, unlike normal red cells that last 120 days, sickle cells are fragile and tend to last only 10-20 days, which usually leads to anemia.
At the present time, there is little that doctors can do to treat sickle cell anemia other than try and manage the complications as they arise. And there is little that alternative health can do to change the underlying condition. However, that does not mean that there is nothing that you can do. It means that it is more imperative than ever that someone with sickle cell anemia do everything they can to optimize the functionality of the blood cells that they have since they have so little margin for error.
Conclusion: the whole is greater than the sum of its parts
In the end, it’s not just individual cells we’re talking about here. Blood is not just the sum of its parts. It’s an integrated whole—an organ, as we discussed in the last newsletter. All the parts interrelate and function as one unit. Each part affects the other.
- Change the pH and you affect the ability of blood to capture oxygen.
- Change the pH and you affect the ability of blood to release carbon dioxide.
- Change the pH in one direction and you shut the immune system down.
- Change it in the other direction and you jack it through the roof.
- Compromise the white cells, allowing bacteria and viruses to remain in the blood (bacteremia and viremia), and you compromise your health—opening yourself up to everything from cancer to rheumatoid arthritis to Crohn’s disease.
- Allow those pathogens to grow in the bloodstream (septicemia) and you die.
- Allow fats to accumulate in the blood and you thicken the blood and cause erythrocytes to clump together—making them more likely to clog in narrowed arteries (i.e., heart attacks).
Again, it comes down to the Baseline of Health®. You need to clean out everything that’s toxic and antagonistic to your body, and you need to provide your body with all the nutrients and building blocks it needs in the forms that can be utilized by the body’s cells. You need to detox regularly. Your exposure to toxic metals, chemicals and xenoestrogens is non-stop. And taking isolated vitamin supplements that are unusable by your body’s cells, does not make up for a bad diet.
All of the steps that we discussed last newsletter about how to optimize the function of blood, apply yet again when it comes to optimizing the composition of blood.
Things to do
- Exercise dramatically improves the gas exchange capabilities of your blood cells.
- Digestive enzymes play a major role in breaking down the foods we eat into forms that are easily transported in our blood and that are easily utilized by our cells.
- Proteolytic enzymes help eliminate circulating immune complexes, which significantly relieves the allergic burden on your body, thus taking a great deal of burden off of your blood. They also quickly optimize the quality of the blood—unclumping it, making it less sticky—thereby improving its ability to transport oxygen
- Sugar metabolic enhancers prevent glycemic swings and help maintain proper sugar levels in the blood.
- Blood cleansing optimizes the performance of the blood.
- Liver cleanses reduce fats in the bloodstream. Keeping the liver clean and balanced is essential to maintaining proper cholesterol levels in the blood.
- Kidney flushing helps the kidneys regulate blood fluid levels and helps regulate EPO hormone levels.
- Supplementation: Every single blood cell in your body is replaced every 120 days. You cannot build the same quality blood cells out of pepperoni pizza, beer, and Ding Dongs that you can out of real food. The ability of blood to clot properly is dependent on having the proper vitamins and minerals (such as vitamin K) present in the diet. If they’re not present in the diet, then you must supplement.
- Immune enhancers and pathogen destroyers help control bacteria and viruses in the blood that tax the immune system.
- pH balance: Our bodies have developed a system for maintaining pH balance in all of our body fluids. To understand this system better, we need to take a look at what changes pH (usually making us more acid), and how our bodies respond to that change. When they are metabolized, carbohydrates, proteins, and fats produce various acids in our bodies. Proteins produce sulfuric acid and phosphoric acid. Carbohydrates and fats produce acetic acid and lactic acid. Since these acids are poisonous to the body, they must be eliminated. Unfortunately, they can’t be eliminated as acids through the kidneys or large intestine as they would damage these organs. How Can We Help?
- Change your diet. Follow the guideline laid out in Chapters 6 and 7 of Lessons from the Miracle Doctors.
- In addition, there are several special alkalinizing agents available.
- Your health food store has alkalinizing teas or drops available.
- There are machines from Japan that will “micronize” your water. What it actually does is take your tap water and divide it in two. One stream is acidic and can be used for washing and cleaning. The other stream is alkaline and is used for drinking. It works really well. Unfortunately, it’s really expensive—about $900-1,200.
- One of the best alternatives is to simply magnetize your water. Applying a magnetic field to a pitcher of water for a short period of time will make it more alkaline, depending on its mineral content. It also offers the added advantage of lessening the surface tension of the water, which makes the water wetter and more usable by the cells of your body.
- Hydration: Dehydration contributes to both thickened blood and edema at the same time. You get the worst of both. Bottom line: you want to properly hydrate…and you want to cut down on excessive use of diuretic drinks such as coffee, tea, and many sodas.
That’s it for now. In the next issue of the newsletter, we’ll explore blood types and how they relate to health—and yes, diet. And we’ll also look at some of the blood tests your doctor runs on you and what they mean.
Read more about Cardiovascular Health
- Part 1 – Blood of my blood
- Part 3 – Blood of my ancestors
- Heart Health Program: Heart Disease Prevention











plasma volume from whole
plasma volume from whole blood collect ?
I truly appreciate this post.
I truly appreciate this post. I have been looking all over for this! Thank goodness I found it on Bing. You’ve made my day! Thanks again!