Today, we begin our exploration of the endocrine system. In many ways, the endocrine system can be viewed as a partner, or complement, to the nervous system. Whereas the nervous system uses nerve impulses that last milliseconds to control short term events in the body, the endocrine system uses hormones that can sometimes take minutes, hours, or even days to take effect and control events. And sometimes those effects can last a lifetime.
Once you understand how important the endocrine system is in controlling every aspect of your life, from your moods to your sexuality to your energy levels to your ability to grow and be strong, you realize how important it is to keep it optimized. And yes, there are things you can do to keep it optimized.
Introduction
The endocrine system is comprised of a group of ductless glands that secrete hormones directly into the spaces surrounding their cells. From there, the bloodstream picks them up and circulates them throughout the body — ultimately reaching the organ or cells designed to respond to a particular hormone. It is the ductless nature of the glands that defines them as part of the endocrine system. As for hormones, they are the body’s chemical messengers that tell the body what to do…and when. Hormones produced by the endocrine system are necessary for normal growth and development, reproduction, and maintaining bodily functions (homeostasis). In humans, the major endocrine glands are the hypothalamus, pituitary, pineal, thyroid, parathyroids, adrenals, the islets of Langerhans in the pancreas, the ovaries, and the testes.
Secretion of hormones in the endocrine system is controlled either by regulators in a particular gland that detect high or low levels of a biochemical and inhibit or stimulate secretion or by a complex mechanism involving the brain, the hypothalamus, and the pituitary.
It should be noted again that the nervous system and the endocrine system are complementary — both in terms of form and function. Both systems share a primary function of coordinating the activities of the body’s many systems. For example, the nervous system tells muscles when to contract and relax, whereas adrenalin tells the body how to respond to stress or threats. The primary difference is that nerve impulses execute their effect in milliseconds…and the effects tend to be short-lived. The endocrine system, on the other hand, takes substantially longer for hormones to wend their way from the gland that produces them, through the bloodstream, and ultimately to the organ or cells where they take effect. In addition, the actions of hormones are much longer lasting than the milliseconds of nerve impulses. Another way of putting this is to say that the nervous system directs the body’s short term responses, whereas the endocrine system directs the body’s longer term responses.
One other point of note is that both systems are mutually interconnected. For example, when the nervous system needs to control things longer term, it acts through the endocrine system by stimulating the release or inhibition of hormones themselves from the endocrine organs. On the other hand, adrenalin, released by the adrenal glands, acts upon the brain to stimulate the fight or flight response.
General definitions
Before we continue, we need to lock down some important definitions.
- As mentioned above, endocrine glands (endo = “within”) are glands that secrete directly into the spaces around the cells and whose products are picked up and circulated by the bloodstream.
- In contrast to the endocrine glands are the exocrine glands (exo = “out”, krinein = “to secrete”). Unlike endocrine glands, exocrine glands secrete into ducts, which in turn, carry the secretions out of the glands and into the lumens (the inner cavities of a tubular organ such as blood vessels and the intestinal tract) or other body cavities or even out of the body. By an overwhelming majority, most glands in the body are exocrine glands, and most exocrine glands secrete their “products” outside of the body. These include sweat, oil, and mammary glands. (We will not be discussing the exocrine glands in this particular series of newsletters.)
- The endocrine system includes some organs that are wholly endocrine in function such as the pituitary gland, thyroid gland, parathyroid gland, adrenal glands, and pineal gland. (It is these glands in particular, along with the pancreas, that will be the focus of this series of newsletters.)
- Endocrine organs that have other functions as well as endocrine functions include the pancreas, liver, ovaries, stomach, hypothalamus of the brain, small intestine, kidneys, testes, and placenta. These are compound glands/organs. (Most of these will be covered when we explore their other functions.)
Endocrine gland locations
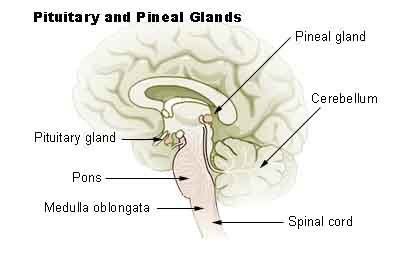
- The hypothalamus, pituitary gland, and pineal gland are located in the brain.
- The thyroid gland is located in the neck, with the four parathyroid glands situated behind it.
- The thymus is in the chest (will be covered when we discuss the immune system).
- The adrenal (AKA the supraneal) glands lie on top of the kidneys.
- The pancreas, stomach, ovaries, and testes are located in and beneath the abdominal cavity and have multiple functions — some of which include endocrine functions.
Hormones
As we mentioned earlier, the endocrine system releases chemical messengers called hormones (hormone = “urge on”), which act on other organs in different parts of the body. Effectively, hormones are the body’s chemical messenger system — they tell the body what to do and when. Some hormones promote or inhibit nerve impulses, while others (epinephrine and norepinephrine, for example) may act as neurotransmitters themselves in certain parts of the body. Then again, these hormones act as hormones (rather than as neurotransmitters) in other places. (This will be much easier to understand when we explore the adrenal glands in a subsequent newsletter.)
Also, as we mentioned earlier, hormones may take seconds, minutes, or hours to work their effects, and their duration of action may be short- or long-lived. How long?
Consider that once estrogen tells a fetus to become a girl, the effect lasts an entire lifetime — unless a doctor intervenes at some point. In general, though, hormones regulate growth, development, reproduction, metabolism, mood, and tissue function.
General properties of hormones
Although they may reach all the cells of the body via the bloodstream, each of the 50+ hormones in the human body affects only a tiny handful of very specific cells. This selectivity is key to the functioning of the endocrine system. How is it accomplished?
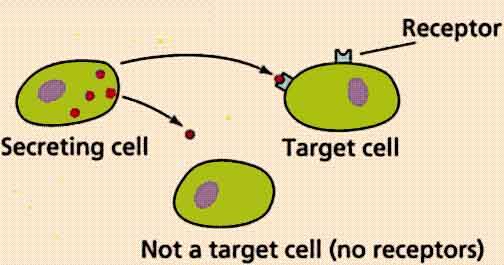
- Target cells contain highly specific receptors, which are surface glycoproteins (proteins which include a carbohydrate and a simple protein).
- The geometry of the glycoprotein molecules allows only for very specific hormones to attach to the receptor in the target cell surface. Think of it as a lock and key mechanism. Exceptions include:
- Chemical mimics such as xenoestrogens (petroleum-based hormone lookalikes) and synthetic growth hormones in meat, etc. — which can be potent in amounts as small as a billionth of a gram. These are never good.
- Plant mimics such as phytoestrogens consumed in the diet or in supplements, which can fill receptor sites, making them unavailable to the stronger natural hormones (or chemical mimics for that matter) in the human body. This effect can often be used to advantage to tone down overly strong hormonal responses in the human body.
Each target cell has up to 100,000 receptors for a given hormone. When there is an excess of that hormone, the number of receptors decreases, reducing sensitivity. This reduction of sensitivity is known as “down regulation.” Also, as just explained, chemical and phyto mimics can fill receptor sites on a cell making those sites unavailable to the actual hormones — thus down regulating the cell. Or in the case of some chemical mimics, up regulating them. (Note: cells contain receptors for multiple hormones, not to mention neuropeptides produced by the brain, and other kinds of receptors too. Thus a single cell may actually have millions of receptor sites on its surface.)
If an abnormally low number of hormone molecules is circulating, the number of receptor sites on individual cells will increase to raise the level of sensitivity and thus compensate. This is known as “up regulation.”
Locally acting hormones:
These hormones do not enter the general circulation. There are two types — one of which, in particular, is of special concern to us.
- Paracrine hormones (para = “near”) act on cells next to the secreting cells without entering the bloodstream — just passing through the interstitial fluid between cells.
- Autocrine hormones (auto = “self”) act on the cell that secreted them. These can play a critical role in terms of our health. Cancer cells use autocrine signaling to trigger growth. This means that cancer cells are autonomous. They don’t take orders from other cells in the body. They tell themselves what to do. That’s one of their features that makes them so dangerous.
Now that we have a basic understanding of what the endocrine system is, what it does, and how it works, let’s start making our way down through the body and begin by taking a look at the three endocrine glands in the human brain: the hypothalamus, the pituitary, and the pineal glands.
Hypothalamus
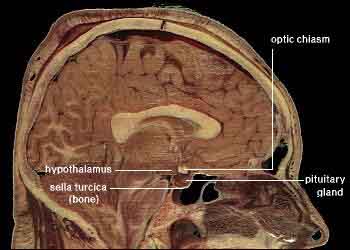 The hypothalamus is located below the thalamus and posterior to the optic chiasm. In humans, the hypothalamus is roughly the size of an almond. But within that small size, it contains a number of small nuclei with a variety of functions. One of the most important functions of the hypothalamus is to link the nervous system to the endocrine system via the pituitary gland. The hypothalamus actually controls the pituitary gland; and it integrates many messages from parts of the brain based on feedback from all over the body and tells the pituitary what to do.
The hypothalamus is located below the thalamus and posterior to the optic chiasm. In humans, the hypothalamus is roughly the size of an almond. But within that small size, it contains a number of small nuclei with a variety of functions. One of the most important functions of the hypothalamus is to link the nervous system to the endocrine system via the pituitary gland. The hypothalamus actually controls the pituitary gland; and it integrates many messages from parts of the brain based on feedback from all over the body and tells the pituitary what to do.
Communication between the hypothalamus and the pituitary is effected through a portal blood capillary system, which connects the two glands over a very short distance. This provides a direct venous to venous connection. The advantage of this type of direct connection is that a portal flow allows blood-borne molecules from the hypothalamus to act on the pituitary before they are diluted with the blood in larger vessels, thus it takes very, very few molecules to direct the pituitary.
The hypothalamus synthesizes and secretes neurohormones, often called hypothalamic-releasing hormones, and these in turn stimulate or inhibit the secretion of pituitary hormones. Among other things, the hypothalamus, through its action on the pituitary, controls body temperature, hunger, thirst, fatigue, childbirth, emotions, growth, milk production, salt and water balance, sleep, weight, and circadian cycles. It is responsive to light (the length of the day for regulating both daily circadian and seasonal rhythms). It is also responsive to olfactory stimuli (including pheromones), steroids, neurally transmitted information (from the heart, stomach, and reproductive system, stress, changes in body temperature caused by infection, and blood-borne stimuli (including leptin and ghrelin (appetite regulating hormones), angiotensin, insulin, pituitary hormones, cytokines, and glucose, etc.)
For the most part, the hypothalamus functions pretty much problem free for the vast majority of people. However, any of the following can cause it to malfunction: anorexia, bulimia, malnutrition, too much iron, bleeding, head traumas, infections, inflammation, genetic disorders, tumors, radiation, and surgery.
Pituitary gland
At one time, the pituitary gland, also called the hypophysis, was once thought to be the “master gland” that controlled all the other endocrine glands. But, as mentioned above, we have since learned that the hypothalamus actually controls the pituitary gland; and it integrates many messages from parts of the brain based on feedback from all over the body and tells the pituitary what to do. In any case, the two glands are tightly integrated. Together, they regulate all processes having to do with primitive reactions, such as stress, rage, flight, body temperature, thirst, hunger, sexual activity, and survival in general. And between them, they secrete 16 hormones.
The pituitary is about 1 cm in diameter, and it lies in the sella turcica (“Turkish saddle”) at the base of the brain, directly behind the optic chiasm. It is divided into two embryologically and functionally different parts: the anterior pituitary and the posterior pituitary. Embryologically refers to what tissue the gland developed “out of” starting as an embryo. The anterior pituitary evolved anatomically up from the floor of the mouth. The posterior pituitary, on the other hand, evolved downward from the base of the brain. In fact, the two parts of the pituitary don’t even talk to each other.
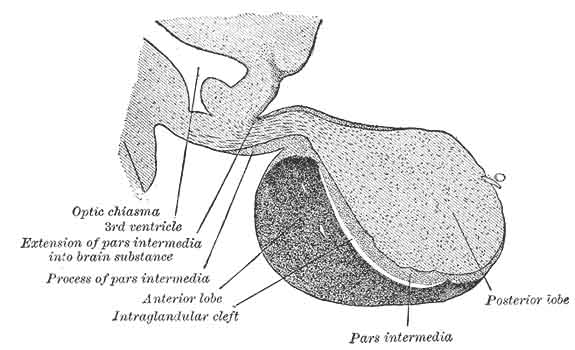
Anterior pituitary
The anterior pituitary gland is also called the adenohypophysis, and it makes up 75% of the pituitary gland — the remaining 25% belonging to the posterior pituitary. Seven releasing hormones (including growth-hormone-releasing hormone and growth-hormone-inhibiting hormone) are secreted by the hypothalamus and are responsible for the release or inhibition of the anterior pituitary hormones. They are generally controlled by negative feedback mechanisms.
Once triggered by the hypothalamus, hormones released by the anterior pituitary flow into the general circulation for action in far parts of the body. Like the hypothalamus, anterior pituitary hormones are also controlled by negative feedback from the brain and the target organ. That is, when the target organ responds to the activating hormone from the pituitary, it will release its own hormone back into the blood, which will travel back to the brain through the circulatory system, which in turn triggers the hypothalamus to turn off production of the stimulating hormone in the anterior pituitary. For example, the pituitary stimulates the thyroid to release thyroid hormones, which travel throughout the bloodstream stimulating metabolism in select parts of the body as required. Through the negative feedback loop, the brain learns that the metabolism has been activated enough (in other words, that enough thyroid hormones have been released) and tells the hypothalamus/pituitary to stop stimulating the thyroid. This completes the negative feedback loop.
Principal anterior pituitary hormones
- Thyroid-stimulating hormone (TSH) stimulates the thyroid gland to release thyroid hormones, which tend to upregulate metabolism.
- Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) together stimulate the release of estrogen and progesterone, which cause the maturation of ova in the female and sperm cells in the male, as well as the release of testosterone.
- Prolactin (PL) stimulates the production of milk by the breasts. As a side note, prolactin can cross the placenta-blood barrier, causing “witch’s milk,” or milk production from a baby’s nipples.
- Adrenocorticotropic hormone (ACTH) stimulates the release of adrenal cortical hormones by the adrenal glands.
- Melanocyte-stimulating hormone (MSH) causes increased skin pigmentation.
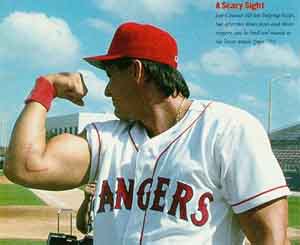
- Human growth hormone (hGH, or somatotropin) stimulates body growth and regulates metabolic processes. High hGH increases the growth of the skeleton during childhood, and it maintains muscle and skeletal size in the adult. Since hGH is probably the best known hormone produced by the pituitary — and in the news constantly because of its illegal use among amateur and professional athletes looking for a competitive edge — let’s take a look at this particular hormone in a little more detail.
Human Growth Hormone
The rejuvenating powers of growth hormone (GH) are no secret to the wealthy and professional athletes: for the last 30-40 years, GH has been available from doctors, requires two injections a day, and costs up to $1,800 a month. Over the last few years, however, several alternatives for the rest of us have become available. And while I could never recommend the injections (for a variety of reasons), I can endorse the alternatives. Many fantastic claims are made for the effects of growth hormone, even claims of “almost” eternal youth. Would that it were so! Although the effects are more subtle for most people, they are nevertheless wide ranging:
 Fat loss (14 percent on average after six months, without dieting)
Fat loss (14 percent on average after six months, without dieting)- Elimination of cellulite
- Higher energy levels and enhanced sexual performance
- Regrowth of heart, liver, spleen, kidneys, and other organs that shrink with
- age
- Greater heart output and lowered blood pressure
- Improved cholesterol profile, with higher HDL (“good”) cholesterol and
- lower LDL (“bad”) cholesterol
- Superior immune function
- Increased exercise and athletic performance
- Better kidney function
- Stronger bones
- Faster wound healing and recovery from injury
- Younger, tighter skin
- Hair regrowth
The most important function of GH, however, is telling the liver to produce insulin-like growth factor 1 (IGF-1), the main key to anti-aging. Specifically, the benefits of GH can be measured in terms of how much it increases the body’s production of IGF-1 (above a 20 percent increase starts to be significant
in terms of effectiveness).
There is some concern that, because it increases IGF-1 levels in the body, GH may increase the risk of prostate cancer. A simple reality check, however, calls these observations into question. First, both GH and IGF-1 levels decline as we age, yet the incidence of prostate cancer increases as these levels decline — the exact opposite of the expressed concern. In addition, in numerous studies involving thousands of patients receiving growth hormone over many years, there were no observed increases in prostate cancer. In fact, based on real-life observation, there is evidence that growth hormone supplementation may reduce the risk of prostate cancer.
Supplementing with Growth Hormone
Most supplement formulas will increase IGF-1 levels by a minimum of 20 percent, with some even approaching 100 percent. But keep in mind that just one 30-minute aerobic session can easily increase IGF-1 levels by 100 percent, and a solid session of weight training can increase levels by an incredible 400–800 percent. Injections, on the other hand, which work directly on the liver (almost like a massive “pulse”), can increase IGF-1 production by only 20–40 percent. A downside to injections, in addition to cost, is that they can give too much GH to the body, shock the body, and can stop the pituitary from producing its own GH. This may explain why injectable GH produces more immediate results, yet ultimately plateaus in terms of effectiveness.
Incidentally, you can no longer actually buy true hGH or human growth hormone. Technically, only growth hormone actually taken from human beings can be called “human” growth hormone. Thirty years ago, the sole source of growth hormone was human cadavers, but that was abandoned when it turned out that growth hormone taken from people had a major downside (in addition to cost) — it occasionally caused the human equivalent of mad cow disease.
Fortunately, at around the same time, recombinant DNA technology came into its own and scientists learned how to alter the DNA of a single-cell yeast plant, and more recently from bacteria, so that they could produce large amounts of growth hormone (molecularly identical to real hGH), safely and inexpensively. Because this growth hormone is identical to hGH, people often use the terms growth hormone and human growth hormone interchangeably, but it should be referred to as a “plant-based growth hormone.”
Given this good, inexpensive source of growth hormone, another problem remained: the growth hormone molecule is so large (containing 191 amino acids) that it cannot be absorbed orally. That meant it could only be administered by injection, which required a doctor and was very expensive. Because of the cost, growth hormone injections became known as the secret youth formula of movie stars, athletes, and the very rich.
For most people, then, the best alternative to GH injections is the use of amino acid-based precursor formulas (also called a GH secretagogues). Typically, these formulas contain ingredients such as glutamine, tyrosine, GABA, arginine, and lysine. Although not as powerful as growth hormone injections, these formulas can be quite effective, provided your pituitary is functioning well, and they carry none of the downside of injections.
Things that sometimes go wrong with the anterior pituitary gland
Not surprisingly, since the pituitary is so involved with regulating growth, some of the key problems associated with a malfunctioning pituitary are related to growth. These include:
 Pituitary dwarfism: Low levels of hGH during the growth years causes bone-growth-plate closure before normal size is achieved. Also, many organs are smaller than normal, and the person has a childlike stature. Fortunately, injections of synthetic hGH produced by recombinant DNA technology in bacteria can prevent this if diagnosed in time.
Pituitary dwarfism: Low levels of hGH during the growth years causes bone-growth-plate closure before normal size is achieved. Also, many organs are smaller than normal, and the person has a childlike stature. Fortunately, injections of synthetic hGH produced by recombinant DNA technology in bacteria can prevent this if diagnosed in time.- Pituitary giantism: Hyposecretion of hGH during childhood causes long bones and tall stature but otherwise normal proportions.
- Acromegaly: Usually caused by functioning pituitary tumors in the already normal adult, it causes thickening of bones of the face, hands, and feet (bones can get longer after the closure of growth centers) and thickening of the tongue, eyelids, and nose. Andre the Giant, the well known wrestler and actor, was one of the world’s best known examples and was, in fact, often billed as The Eighth Wonder of the World. Another famous (possible example) might have been the biblical Goliath, who was slain by David with a slingshot. In fact, there is a very interesting theory, with real scientific basis, that proposes that Goliath’s acromegaly might actually account for how he was slain by David. According to the theory, a pituitary tumor, because of the pituitary’s placement right behind the optic chiasm, can sometimes place pressure on peripheral vision nerve fibers, resulting in tunnel vision. If Goliath had that condition, which sometimes does occur with acromegaly, he would have been blind to David, if David approached from the side, and a rock hurled from the side would hit the temple at the thinnest part of the skull, thus stunning the giant. Once stunned and on the ground, David would then be able to safely approach his now helpless victim and cut off his head. And thus the legend was born — or so the theory goes.
Posterior pituitary gland
As I mentioned earlier, the posterior pituitary gland (AKA the neurohypophysis) is anatomically derived from a down growth of the brain and is not technically a gland since it does not synthesize hormones, but rather, stores and secretes two hormones actually made in the brain. These two hormones, oxytocin and vasopressin, are transported from the brain in small packets for storage in the posterior pituitary — to be released as needed.
- Oxytocin (oxytocia = “rapid child birth”; AKA Pitocin) enhances the strength of uterine contractions and stimulates the ejection of milk after delivery. It may also foster maternal instincts and sexual pleasure during and after intercourse. Now synthesized and readily available, it is often given to women to help them have stronger contractions and expel the fetus in a more timely manner…when necessary.
- Vasopressin (Antidiuretic hormone, ADH) decreases urine production by increasing re-absorption by the kidneys, a useful trick when suffering from dehydration. The effect, though, is to raise blood volume and, therefore, to raise blood pressure. Alcohol inhibits ADH secretion, thus producing profuse urination after a drinking binge, which leads to severe dehydration, and the severe dehydration leads to the headache and thirst associated with a hangover.
Pineal Gland
The pineal gland is about the size of a grain of rice, is shaped like a tiny pine cone (hence its name), and is located in the center of the brain in a tiny cave, behind and above the pituitary gland. For years, mystics considered it to be the seat of the mystical third eye, whereas the medical community considered it vestigial and, thus, pretty much non-functioning. Since then, the mystics have not necessarily been refuted, but the medical community has been. The pineal gland is now known to be the major source of melatonin production in the body. It is full size in children, a size it maintains throughout adulthood — although its weight can drop significantly starting with puberty. And it is not unusual for the gland to literally calcify in many adults. The gland most likely plays a significant role in sexual maturation, circadian rhythm and inducing sleep, and in seasonal affective disorder and depression. In animals, it plays a key role in hibernation.
Melatonin
The trigger for production and release of melatonin is total darkness — any light in the room will inhibit this process. Today, however, living in a world with nightlights in the bedroom or streetlights sneaking through the window, we actually have an epidemic of people with insufficient melatonin production, even at a very young age. The problem doesn’t just come from light falling on our eyes while we sleep, but from light falling on any part of the body. Even if you wear an eye-mask, if any light is falling on your arms or chest or feet, that’s enough to slow melatonin production. Without artificial light, we would normally be in total darkness 8–12 hours a night, producing melatonin during all of those hours. Living in a city or suburban area may cut the hours of total darkness to six or less, and in many cases, zero. Melatonin levels also decline significantly as we age. Since its discovery in 1958, melatonin has been studied extensively and shown to be widely beneficial to the body. The benefits of supplementation to compensate for abnormally low production in the body include:
- Better Sleep — Lowered levels of nighttime melatonin reduce the quality of sleep, resulting in the need for more sleep. If your pineal gland does not produce adequate melatonin early enough in the evening, both the quality and quantity of your sleep may suffer. Lack of melatonin may make it difficult for you to fall asleep or may cause you to wake up too soon. Too much melatonin and you will feel exhausted or “drugged” throughout the day. By taking melatonin instead of other sleep aids, rapid eye movement (REM) sleep (dreaming) is not suppressed nor does it induce “hangover” effects when used as directed.
- Enhanced Immune Function — Many people report that supplementation with melatonin has significantly reduced their incidence of colds and infections. The exact way in which melatonin affects the immune system is not known. However, since much of the activity of the immune system takes place at night, some researchers have proposed that melatonin interacts with the immune system during sleep, helping to buffer the adverse effects of stress. It has been proposed by some that the increased incidence of cancer we see today is partially due to the extended time we are exposed to artificial lighting. This is reflected in the fact that melatonin levels in breast cancer and prostate cancer patients are half of normal.
- Powerful Antioxidant Capabilities — Melatonin is one of the most powerful antioxidants produced in the body. In addition, since it is both water and fat-soluble, melatonin can reach almost every cell in the body. However, since it cannot be stored in the body, it must be replenished daily.
- Mood Elevator — Nighttime melatonin levels are low in people with major depressive and panic disorders. Individuals with mood swings or who are melancholic also have lower melatonin levels. Both seasonal affective disorder (SAD) and cyclic depressions are related to the peaks and valleys of melatonin levels.
Third eye
While the physiological function of the pineal gland remained unknown until recently, mystical traditions and esoteric schools, have long considered the pineal gland to be the connecting link between the physical and spiritual worlds…and the seat of extrasensory perception. I am not here to argue the spiritual qualities of the pineal gland, nor talk about its extrasensory capabilities, excepting one: its sensitivity to light.
As medically theorized, the pineal gland responds to the ebbs and flow of light entering our eyes during the day. In the evening, the pineal gland reacts to the diminishing levels of daylight and starts to produce melatonin, which is then released into the blood and flows through the body making us drowsy. Its secretion peaks in the middle of the night during our heaviest hours of sleep. In the morning, bright light shining through the eyelids reaches the pineal gland which reacts by switching off the production of melatonin, thus removing the desire to sleep. And we wake!
But this description is incomplete in one significant aspect. As it turns out, the pineal gland can be diminished not only by light shining on the eyelids, but by light shining anywhere on the body. Literally, light striking any part of your skin can reduce production of melatonin from the pineal gland. It seems the pineal can “see without eyes.” How’s that for ESP? Even more interesting is the fact that in some lower vertebrates the pineal gland actually has a well-developed eye-like structure and is considered by some scientists to be the evolutionary forerunner of the modern eye. In other vertebrates, though not organized as an eye, it functions as a light receptor — effectively a third eye.

In any case, the key when it comes to the pineal gland and melatonin is that it’s important to sleep in a darkened room, with no light coming through the curtains or night lights turned on in the room. And wearing eyeshades won’t help as the pineal can sense any light shining on your skin. Failure to sleep in a darkened room will inhibit melatonin production, which presents a series of health problems, not the least of which is an inability to sleep deeply. But beyond that, if continued for too long, it will literally shut down the pineal and cause it to atrophy. At that point, your only choice will be to use melatonin supplements.
Conclusion
We’ll pause here and pick up our discussion of the endocrine system in the next newsletter with an exploration of the thyroid and parathyroid glands. One of the interesting things you’ll notice is that as we move down through the body, you’ll find that you have progressively more options for altering the behavior of your endocrine glands. That said, you can nevertheless consider using the following supplements to assist the hyopthalamus, the pituitary, and the pineal glands in the optimal performance of their basic functions.
- hGH secretagogue — available throughout the internet
- Timed release melatonin
- Hypothalamus PMG from Standard Process — available throughout the internet
- Pituitrophin PMG from Standard Process — available throughout the internet
Enjoy the following links to complete the entire newsletter series on the Endocrine System:











Neat. Discribtion. Very.
Neat. Discribtion. Very. Benificial
I would like to receive this
I would like to receive this news letter.
.
Click here: http://jonbarron
Click here: http://www.jonbarron.org/subscribe-our-free-bi-weekly-health-reports
This has been incredibly
This has been incredibly instructional, to the point, and invaluable information for someone who is trying to rehabilitate the hypothalamus gland.
It was like being in the classroom with a great lecturer, easy to understand, informative and entertaining.
Thank you!
I'm very grateful with your
I’m very grateful with your newsletters and specially this one since I’m trying to improve the function of my endocrine system. You indicate that we can get throughout the internet the hgh secretagogue but there is a problem they have so many that I don’t know which one is better also I tried to get the hypothalamus PMG and the pituitropin PMG from Standard Process and they don’t sell them to the public you have to provide them a zip code where you live and they refer you to a professional facility to take care of you and I don’t like that. Can you help me please? 1- Which is the best hgh secretagogue 2- There is another way to get the hypothalamus PMG and the pituitropin PMG. I will appreciate to hear from you.
Thank you in advance
MHP Gold is a reasonable
MHP Gold is a reasonable secreatgogue. And you can get it at a good discount from vitacost.com. As for Standard Process products, it’s true they don’t sell directly to the public. But you can buy them on Amazon.com.
I notice that there doesn't
I notice that there doesn’t seem to be any information in this article about the homeopathic GH described in “Lessons From The Miracle Doctors.” Does this mean that the homeopathic GH has been shown to be ineffective?
Also, is there a rule-of-thumb trial period to see some results for either the secretagogues or the Standard Process Hypothalamus PMG and Pituitrophin PMG?
Thanks, as always, for a very clear and informative article; I recommend your newsletter to everyone interested in real health.
It’s just that, over time,
It’s just that, over time, Jon has determined that for most people secretagogues are the best option. Also, in terms of homeopathic supplements there has been such a turnover in products and companies over the yearts that Jon couldn’t keep up with them, and therefore could not make any recommendations as to which products worked and which did not.
What would a cyst on the
What would a cyst on the pineal gland do to it? Would it cause more or less melatonin to be produced, or not harm the pineal’s function at all? Could a pineal cyst, if large enough, cause pressure to the hypothalamus or disturb th communication between the pineal and other endocrine glands?
Pineal gland cysts are common
Pineal gland cysts are common affecting 1-4 percent of healthy adults. In older adults, as evidenced in autopsies, the numbers range from 21-41 percent. They are generally benign and only rarely cause symptoms. That said, if the cysts become sufficiently large – greater than a half centimeter, which is extremely rare — they can cause headaches, vision problems, sensitivity to light, disruption of the body’s daily cycles, and even swelling in the brain.
Surgery is sometimes an option for large cysts. There are no proven natural treatments, but detoxing would probably be a good place to start – especially heavy metal detoxing as the pineal gland is extremely sensitive to mercury.
Hello. My two year old has a
Hello. My two year old has a pineal cyst over 1cm that is symptomatic and putting pressure on the hypothalamus. What is your opinion on what this pressure could do to the endocrine system?
For obvious legal reasons, we
For obvious legal reasons, we cannot diagnose or prescribe for specific medical conditions—merely provide information. With that said, perhaps the following article will be helpful.
http://www.jonbarron.org/article/endocrine-system-hypothalamus-pituitary-pineal-glands#.VGpSu9GBFxQ
worthy,thanks
worthy,thanks
I have a pineal cyst
I have a pineal cyst 12by10by9mm with a novel of symptoms, from balance and coordination, memory, visual disturbances, sleep issues, head pressure, headache, dizzy, nausea, ataxia, speech problems, cognitive dysfunction, and many more. I’ve seen nearly two dozen Dr’s. all of which blow me and the cyst off. I’ve passed numerous tests with flying colors, andDr’s have no answers except for what I DON’T have, and refuse toacknowledge the cyst as a problem. do you have any suggestions? I’m running out of options, and miss being my old self. I would jump at the chance to have this removed, but again have been dismissed by the medical community. any suggestions are appreciated!! I can’t take the pain and suffering much longer!!
Hi – interesting that you
Hi – interesting that you posted this just a few days ago. I was diagosed with a pineal cyst several years ago. Had other cognitive/memory/etc., thus put it on the bottom of the concern list. However, I have a host of issues going on which involve the endrocrine system – hence, recalling pineal cyst issue.
First of all, I googled pineal cyst yesterday and found that there is a new technique for pineal cyst removal – if deemed necessary. I’m sorry, but I don’t remember what the technique is called – think that it’s an endoscopic technique. I’ll check my history to see if I can find the link for you. . I also have many of your issues listed and have had many of them for 15 years plus. It’s very confusing, for I am also psychiatrically ill and have been reacting from long-ago prescribed medicines, hypothyroidism, high cholesterol levels, etc., which makes the situation all the more confusing. Which came first…
I have a great endocrinologist who is leaving no stone unturned. Ordered a huge amount of blood work. Bone density scan, thyroid ultrasound and carotid ultrasound. Am actually glad that he did. Have you tried an endocrinologist? Pineal, pituitary, etc., all work together…perhaps there is something else going on? (It sounds as if you would already know this, considering the number of docs you have seen.) I’m sorry for mentioning what you probably already know. Oh…are you/have you seen a doc – specifically an endocrinologist – at a teaching/university/medical school? I have found the best doctors at such locations. There are many not associated, of course, but I just thought that I’d toss out that suggestion.
The reason I’m telling you this is that my hypothyroidism has been stable for 20+ years. Suddenly, it’s way off. Weirder yet, is that I’ve unintentionally dropped over 20 lbs in two months. (Huh-typically would be gaining weight!) The pounding headaches are terrible and relentless – as yours are most likely. The symptoms go on and on. Frustration!
Next question…have you tried OTC melatonin? As you know, the pineal gland is directly correlated with melatonin – perhaps supplementing your diet with melatonin might give you a little relief/regulate your sleep as you’re trying to figure out the issues. It takes a little while to “get in your system” – don’t remember how many days. However, from what I’ve heard, it’s harmless and is definitely worth a try.
Anyway, I’m searching and searching as you are. Will bookmark this page and let you know if I find anything helpful. Hang in there!
Feel better –
Polly
melatonin and I don’t agree,
melatonin and I don’t agree, if anything, I have excess melatonin symptoms (which one discovered is typically more associated with tumor over cyst), and every time I take any melatonin, I have horrid nightmares, night sweats, am more tired and groggy than not… It’s awful!
I’ve seen nearly 2dozen Dr’s, endocrinologist included. all my blood work can’t back near perfect and he was stumped. He tried to blame some of my issues on other things that don’t make any sense.
Dr’s don’t consider 30% growth in 7 months as important, they just say it’s insignificant. mine doesn’t look like everyone else’s typical cysts,either. It’s not dark in the center, it looks more like brain matter, which makes me wonder if it’s a pinocytoma instead. However, because I don’t show hydrocephalus, noone here in the states will touch me. I’ve found surgeons in Finland and Australia I’m waiting to hear back from for approval, but it’s so frustrating,painful, etc… I’m so tired of being told by Neuro’s that I’m making it up, my symptoms aren’t neurological, that I’m not actually feeling what I’m feeling, and that I’m basically crazy. I can’t believe the deny-avoid concept they all have regarding this! I was told if it grew, then they would consider it…Well, it grew and now I get – it depends on the slice, who measured it, etc… let’s try again in 3months. why? what’s the point? It’ll STILL depend on the slice, who measured, if their grandmother’s goldfish died that day, etc.
I know Ihave endocrine issues, but they aren’t doing anything about it. I’m more than convinced it’sthis cyst causing my issues, is the only abnormal thing in any testing thatbe been found and the symptoms fit. Ugh. stupid Dr’s….
I know that this is going to
I know that this is going to sound crazy but it is the truth. In September 2008, I saw a chiropracter that did a adjustment by pulling straight out on my neck instead of side to side. My neck popped and if felt better. With in 5 days of this all of a sudden My smell improoved 100% and the FAT STARTED JUST FALLING OFF OF ME, BUT I HAD MUSCLE. I FELT BETTER THAN I HAD SINCE I WAS IN MY TEENS. AT THE TIME I WAS 42. Could that have triggered my pituitary gland and made it work again some how. I felt so great that I did not go back and sadly after a year everything started going down hill again and I am so desperate to find a chiro- who does this kind of adjustment. Any help would be soooo APPRECIATED. THANK YOU
It sounds like a version of
It sounds like a version of an occipital lift. It’s unlikely it had anything to do with the pituitary. Instead, an occipital lift relieves muscular dysfunction in the suboccipital triangle, thus resetting muscle tone, while at the same time producing a normal realignment of the vertebrae in the neck, which relieves tension and reinvigorates nerves throughout the head and face (think improved sensory function).
I wanted to know about the
I wanted to know about the advantages and side effects of combining steroids with a gym routine?
As I am sure you know,
As I am sure you know, steroids are powerful drugs and have serious side effects. Jon would never recommend them, especially to just enhance your fitness. Have you looked into an alternative route for athletic performance that will actually boost your immune system? You should check out our natural athletic performance program.
Does taking melatonin make
Does taking melatonin make the pineal stop producing it altogether? I’m concerned about causing the pineal to atrophy as you mentioned can happen.
Taking supplemental melatonin
Taking supplemental melatonin does not appear to be a factor in pineal atrophy. Not sleeping in a dark room, exposure to fluoride, and an acid pH, on the other hand, do.
excellent article!
excellent article!
At the age of 10, my daughter
At the age of 10, my daughter developed a large inoperable rhabdomyosarcoma pushing from the temporal fossa on the right side up into her brain right near near her pituitary gland. It ‘miraculously’ disappeared after 12 months of combined chemo/ radiotherapy We also used many natural therapies including herbals , emu oil and shiitake mushroom . I am convinced that these helped her ‘total’ recovery. Unfortunately she has a resulting trismus of the jaw with only about 1/3 of the normal mouth opening and a smaller jaw bone on the right side and some loss of muscle ( although not hugely noticeable at first glance ). She also has reduced growth hormone levels due to radiotherapy- she was on neuropin growth hormone for 18 months as prescribed by the endocrinologist due to little advancement in her growth – . She is now 5foot , 3 inches . I have been told this is pretty much it for her growth as she is now 14 years old and reached puberty – although with inconsistent periods ( even after 2 years) I have been told by the drs that this us ‘totally normal’, and not to worry about this ( or that she is below her expected height which would be approx 167cm)/ she was on the 75percentile for girls her age prior to treatment and now is around the 30-40 percentile . If there are any suggestions , supplements that you could possibly offer to help her in these areas would be greatly appreciated.
Hi Sharon,
Hi Sharon,
Have you read Jon’s book yet? That is where I would start.
Hello, I’ve just discovered
Hello, I’ve just discovered your work, and I am amazed at how Informative it is. I have had a total thyroidectomy in January 2011 due to benign nodules. I regret it to this day as I have yet to feel like my old self. I don’t know exactly what I’m asking other that is there hope to feel again like a normally functioning person? Can another gland take on the thyroid finction? If yes, what can I do about it. Thank you in advance for your answer.
Unfortunately, no other
Unfortunately, no other glands pick up for the thyroid once it’s removed. http://www.jonbarron.org/article/endocrine-system-thyroid-and-parathyroid-gland. You will now need to work closely with you doctor to continually tweak the levels of your thyroid medication until you can finally approximate the levels that were normal for you before the surgery. Don’t let your doctor brush you off if you’re not happy with how you’re feeling. Remember, you’re the one who has to live with it, not your doctor. Finding balance with thyroid medication can be difficult and take many months to finally get something you can live with. But it you work at it, you can get reasonably close.
The Pineal and Pituitary are
The Pineal and Pituitary are not in the brain. They’re actually outside of the brain and an extension of the roof of the mouth.
Do you know where I can find
Does anyone know where I can find further information on Melatonin production being affected by not only light falling on the eyes but the rest of the body also?
Thanks
I am finding myself chasing
I am finding myself chasing answers to puzzling symptoms which have left a good number of specialists baffled.
After acoustic neuroma surgery (right side) 14 months ago, I lost most of my sense of taste. I could hardly taste anything sweet at all, but I started getting a taste of something salty coming from the back of my mouth on the right side of my tongue.
Then I started having difficulty breathing, as if I was drawing breath through a fine sieve or trying to breathe through ammonia fumes. Now and then my right eye would start burning, and the corners would get encrusted with what feels like shards of glass – or it would start weeping. My eyes still dry up at night and I regularly wake up unable to open my right eyelid.
My neurosurgeon, his Nose/Throat specialist assistant, as well as an ENT specialist can’t explain what is happening. Spinal fluid has been ruled out as the site was sealed with fat to prevent such occurrence. I am now scheduled to see an ophtalmologist in January to have my tear ducts checked…
Though an ultrasound performed last week showed my thyroid to be normal, years ago I was diagnosed with hypothyroidism, and the W indentation and scalloped tongue pointed out at the time are still present. There is tightness in that area of my throat. My research here first led me to suspect something wrong with the (parotid?) salivary gland/duct.
Further research pointed to the endocrine system: “Among other things, the hypothalamus, through its action on the pituitary, controls body temperature, hunger, thirst, fatigue, … salt and water balance…”. A few days ago, I woke up with a very strong taste of salt in my mouth which has not abated. Hypothalamus, pituitary gland, optic chiasm (?) also seem like good suspects. If the issue is indeed sodium, what effect is it having on my eyes, brain, etc.?
Maybe I should mention that I have been on hormone replacement therapy for six months and was also diagnosed with PTSD. And finally, my claim to fame: I am Jon’s age!
Like Kirsten, I have run out of options. I am convinced that the likely culprits are being overlooked. Perhaps an endocrinologist would be able to help at this point? Hope you can shed some light on the matter – thank you.
One more thing: my husband and I normally start on Jon’s detox program at this time of year. Would it be advisable to delay our detox this year until this issue has been figured out?
For obvious legal reasons, we
For obvious legal reasons, we cannot diagnose or prescribe for specific medical conditions—merely provide information. In any case, since your symptoms are wide ranging and without any known cause, the best we could recommend would be doing the entire Baseline of Health Program to optimize your body’s ability to correct any imbalances. That said, you might want to find an a natural healer in your area with whom you can work directly.
I’m a male, 58, (look like 40
I’m a male, 58, (look like 40), who maintain a healthy diet with fruits and vegetables and some chicken, (turkey or fish), take daily digestive enzymes, probiotics and drink alkaline water. I don’t smoke, drink alcohol (only socially), or consume processed foods, starches, coffee, sugars, nor drink soda beverages either.
*) Last year, I was diagnosed with a Macro-Adenoma (Benign Pituitary tumor), through an MRI test. I have severe loss of libido, lost interest on sex, very poor or no erections, critically low levels of (regular and free) testosterone (blood test result show 159, when 250 is the minimum).
*) Levels of Prolactin show only 10 points above normal, therefore is NOT considered a Prolactinoma.
*) Bone Density test shows: “Osteopenia” (condition before Osteoporosis) affected on L3, L4 & L5 (lumbar vertebras).
(Since my diagnosis, I’ve incorporated baking soda in water, to maintain an alkaline system).
*) I have an enlarged prostate with PSA levels of 9 (4 is the max).
*) High blood pressure levels (150/98 or higher VERY often).
Tried different several herbal prostate formulas with Saw Palmetto, Beta Sitosterol etc, but I immediately noticed a small “lump” (hard tissue) growing inside my right nipple. The moment I stop, it disappears.
*) I also have a “one-inch” Hiatal Hernia (sliding), diagnosed around 7 years ago.
I’ve had digestive issues since childhood, taking a toll mainly in my intestines.
Very often right after I eat a meal, I feel sluggish and EXTREMELY sleepy, so much so, I would fall asleep “without realizing it” (even though I take digestive enzymes).
Please note the following MENTALS & EMOTIONALS, to help you narrow down the right remedy selection:
One of the main symptoms is mental and emotional “immobility”, as if “chained-up”. Since few years back, I started to feel diminished and scared like a little boy, to make any decisions.
*) Emotional instability
*) Severe problem in making decisions. I feel as if I stuck between two things I can’t decide!
*) Insecure.
*) Easily startled and/or scared.
*) Rapid emotional changes
*) Very poor memory and concentration. Unable to retain a sentence I just finished reading.
*) Impaired judgment
*) Reduced alertness
*) Personality & behavior changes.
*) Very difficult to focus on one thing and quickly jump onto another one without finishing ANY task I’ve started.
*) Confusion
*) Doubting my masculinity at times (due to very low testosterone levels???).
My intention is to avoid this surgery since I’ve personally met several people with similar condition, that they’re now need to be on hormonal meds for the rest of their lives, or others had to have their Pituitary gland entirely removed, due to radiation treatments a while after they’ve had the surgery .
I’ve tried the Banerji protocol (Ruta Grav. & Calc. Phosp) and my tumor grew even 1cm bigger! I stopped immediately.
Please help me in finding the right remedies and how to take them, since I’m even a homeopathy advocate, I still can’t treat myself.
Thank you very much in advance!
Kindest Regards.
I’ve developed a “smell” in
I’ve developed a “smell” in my nose. It first happened about three years ago. The smell was like a forest fire or burning wood. It kept me awake for a full seven days and nights. I almost had a nervous breakdown. It finally went away after an ER visit with no diagnosis. Now I have a different smell, like some sort of “rub” you put on meat before you cook it. It’s driving me crazy. When I eat or drink certain things, I really smell it strong. The things I eat or drink don’t taste the same as I remember them tasting. When I go to sleep, Sleep comes quickly but only lasts about two hours. then I’m awake, asleep, every thirty to sixty minutes throughout the remainder of the night.
Your article is really
Your article is really fabulous. I like your article. What a wonderful article.I gained more knowledge about endocrine gland. Thank you for posting such a wonderful article.I request you to put more information about melanin.