Many, many years ago when I worked for Kaiser Permanente, I came down with a really bad flu and felt miserable. In desperation, I headed off to the Kaiser clinic to see if they could help. After diagnosing the flu, the doctor wrote up a prescription for antibiotics. “Antibiotics,” I blurted out through my fevered haze. “Aren’t antibiotics for bacterial infections? Isn’t the flu a viral infection? How will that help?”
“It won’t really,” he answered, “but you were expecting me to give you something to help, right?”
Since then, I’ve learned that doctors abide by the principal that to be a good physician, you must do something for the patient, whether needed or not. And so we have the common phenomenon of the unnecessary procedure — including unnecessary hysterectomies, unnecessary CT scans, and so on. Now a new entry has just been added to the list of common procedures the patient could have lived without. New research by the Duke University Medical School indicates that a whole lot of cardiac catheterizations are being performed on patients who have no significant artery disease.
The study examined the US national cardiac registry to identify two million people who underwent cardiac catheterization between 2004 and 2008. Of these, 400,000 had stable chest pain without previous diagnosis of heart disease. The catheterization results showed that only 38% of these patients actually had significant coronary blockages. Study director Dr. Manesh Patel comments, “We’re spending a lot of energy and money to evaluate chest pain which often leads to cardiac catheterization, which, we now know, often finds that patients don’t have significant obstructive disease. Our research shows that our methods for identifying patients at risk for obstructive disease need significant improvement.”
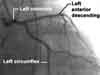
Physicians generally perform catheterizations for diagnostic purposes to identify the presence, location, and severity of coronary atherosclerosis, according to Dr. Patel, as a preliminary step in evaluating if angioplasty (and don’t get me started on angioplasties) or bypass surgery will be needed. The procedure for diagnostic catheterizations involves inserting a tube into a blood vessel in the arm or leg and guiding it to the heart, where it sends information to an x-ray machine. This provides information to locate blockages in arteries, measure pressure and oxygen in the heart chambers, and evaluate the overall health of the cardiovascular system. Catheters also can have balloons attached that inflate to clear arteries — at which point, you’re actually performing a coronary angioplasty. Clearing the arteries in this way can “theoretically” prevent and stop heart attacks.
A case can be made that catheterization is useful as a diagnostic tool when there actually is heart disease and significant blockage of the arteries, but it’s being commonly applied to patients who have neither of these conditions. And there is no justification for that. Again, in almost two-thirds of patients with stable chest pain but no prior heart disease, the cardiac catheterization found no significant artery disease.
If the procedure came without risks, this wouldn’t be a problem other than for the expense and time involved, but the fact is that catheterization is an invasive procedure. Complications can include bleeding, infection, and pain where the catheter was inserted; damage to blood vessels; allergic reactions to the dye used, and in rare cases, the catheter may scrape or poke a hole in a blood vessel as it’s threaded to the heart. More serious, but less common complications include arrythmias, kidney damage from the dye, blood clots that can trigger stroke or heart attack, low blood pressure, and a build up of fluid in the sac around the heart.
It doesn’t help that most patients — 84 percent — first go through supposedly less risky noninvasive procedures like stress tests before catheterizations, to find out if they need the catheterization. But the research concluded that these noninvasive tests have remarkably poor predictive value, and they carry risks of their own. The nuclear cardiac stress test, for instance, blasts patients with an enormous dose of radiation — more than any other diagnostic test, including CT scans. According to Wikipedia, “Stress test results are often falsely negative for many people…It has become clear that stress testing recognizes most people at risk for heart attacks too late, unfortunately only after the disease and symptoms of the disease have developed.” In other words, stress tests carry a lot of risk for questionable benefit.
Dr. Patel says, “Our research shows that our methods for identifying patients at risk for obstructive disease need significant improvement.” He adds that the whole process for caring for patients with heart pain needs to be reevaluated, including how histories are taken, how risk factors are assessed, and the role of diagnostic procedures.
Meanwhile, cardiac catheterization is big business. According to Surgery.com, more than 1.5 million cardiac catheterizations were performed per year, as measured in 2009. The use of the procedure was expected to increase to more than three million by 2010. A 2007 article in diagnosticimaging.com pegged the cost of a typical cardiac catheterization at about $10,000. In 1990, about $4.5 billion was spent in the U.S. to perform about 1,000,000 cardiac catheterizations. Add to that the price of preliminary stress tests, and you’ve got a lot of money being spent for nothing, and a lot of people undergoing diagnostic testing that might create problems where there were none.
Then again, like my flu doctor, it is a way for your doctor to make you feel he’s done something (even if there’s no benefit), assuming that’s all you’re looking for. And besides, it’s free — paid for by your insurance company.
:hc










Soooo!!!!! What do you do, if you do have problems with your heart…is there any other way finding out if you do have blocked arteries, and how do you overcome the problem??
So what is the answer? One third of the patients did have significant blockage and may have had their lives saved. I don’t like your attitude in comparing this test to needlessly prescribing antibiotics. Lives were saved and I don’t see you offering an alternative way in which these sick people would have been diagnosed. And no I am not a doctor.
I buy a lot of your product,s because I trust you, but sometimes in articles such as this, your anti medical vehemence is so strong that it appears to short circuit your logic. This makes me uneasy and causes me to wonder if youyr claims for your products might also be somewhat tainted by your bias.
Harry:
You seem upset with me, but it was the study director, Dr. Patel, who said, “Our research shows that our methods for identifying patients at risk for obstructive disease need significant improvement.” He adds that the whole process for caring for patients with heart pain needs to be reevaluated, including how histories are taken, how risk factors are assessed, and the role of diagnostic procedures. Just because I’m reporting on the study results is no reason to “”shoot the messenger.””
And yes, one third may benefit, but two thirds are put at risk. If you’re one of the one third that received benefit, you would probably say that it was a worthwhile test. But if you were one of those in the two thirds group that had a major complication, you (or one of your surviving family members) would probably be contacting a lawyer.
I think you do a wonderful job of teaching. I also, like Barbara, am searching for alternatives to clogged arteries. I also agree with Harry that more than research results were in this message. You see, many women have coronary artery disease( as you well know, it is a silent killer) & if there is significant blockage, our only alternative has been angioplasty with stent placement(.By the way, I do have a problem with stress testing on patients presenting with heart problems. I actually had an uncle in-law who had a heart attack this way! ) This is even after exercising, diet watch, & losing weight. I hate the thought that this is our only alternative, not to mention the medications with all the side effects. Therefore, I study the best I can, make choices, & pray for alternatives. Thanks for listening.
Just had pain in upper right chest and right arm ( 5/24/10). went to ER…..nitro & aspirin stopped pain completely…..admitted to hospital heart dept…..called in cardiologist…he ordered angioplasty for 5/26….kidney doc says kidney is too weak (46%) and could be ruined….card doc calls for neuclear stress test….very painful result at area listed above…card doc says we go ahead w/ angio…I say no…he sends me home w/ perscriptions for several meds incding nitro and PLAVIX. (5/29). Read your article 5/31….thank you. I will live w/ the pain and meds.