In our last newsletter, we explored how when it comes to end-of-life medical intervention, physicians pretty much take a “Do as I say, not as I do” approach–as they overwhelming reject the same medical procedures they recommend for their patients. In this issue, we’ll take a look at how they stack up when it comes to diets. Today, because of the overwhelming levels of obesity in the United States, Australia, much of Europe, and even the developing world, physicians are supposed to counsel their patients on how to modify their diets to lose weight and achieve better health. The results of that counseling pretty much speak for themselves: not very successful. Which leaves us with the question: is the failure a result of doctors not following their own advice and, thus, having no credibility with their patients, or does it lie elsewhere? In fact, as we will see, the reason medical doctors do not make great dietary counselors stems from the fact that, quite simply, they are as confused as the rest of us. They don’t really know what to recommend, don’t really understand the essence of proper diet themselves, and therefore, make a mash of the job when trying to explain proper diet to their patients. And, as we will see, this should not really come as much of a surprise.
Let’s start by taking a look at a recent Medscape survey asking physicians about their lifestyle choices and, particularly, what diets they do follow.1 Carol Peckham. “Medscape Physician Lifestyle Report 2014.” January 23, 2014. Medscape. http://www.medscape.com/features/slideshow/lifestyle/2014/public/overview#1 Then we’ll discuss what it means and what you should do in terms of a healthy diet.
What diets do doctors follow?
All of the key information in the survey is summarized in the following chart.
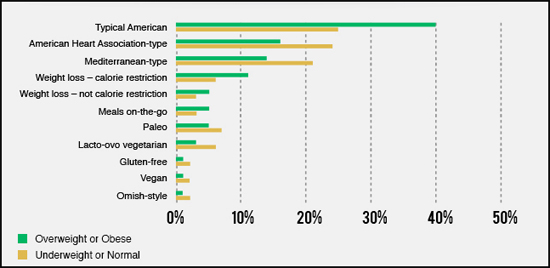
What leaps off the page is the fact that, far and away, the largest number of physicians eat some combination of the typical American diet and meals on-the-go–which is the same thing, only prepared by other people. Although, they may eat less fast food than the average person, we’re not talking healthy dining. Most physician meals on-the-go are sit-down meals at mid-level restaurants and chains. Even worse, this is especially true for those docs who are either overweight or obese–with just under 50% of those docs eating badly. Obviously, the dictum “Physician, heal thyself” has not been widely adopted in the medical community. To be clear, what we’re talking about here is the typical American Diet which can be defined as meat and carbs–in the form of potatoes, rice, and bread. This is not the “meat lovers” diet that restricts carbs–sometimes referred to as the Atkins diet, or in its more refined form, the Paleo diet. This is the typical, unhealthy American diet. Also notable is the fact that only 16% of overweight and obese doctors are on a weight-loss or calorie-restriction diet. With what credibility can such doctors tell you to have the willpower they can’t summon up?
Let’s quickly touch on the different diets identified in the survey and then take a look at what it all means.
- Typical American
- American Heart Association
- Mediterranean
- Weight-loss, caloric restriction
- Weight-loss, no calorie restriction
- Meals on-the-the-go
- Paleo
- Lacto-ovo vegetarian
- Gluten free
- Vegan
- Ornish
Typical American
As already stated, the typical American diet, as defined in this survey, refers to a meat and potatoes diet–not particularly health oriented. It is high in fats, sugars, and starches and contains very few fresh fruits and vegetables. It is the diet now sweeping through much of the third world and is strongly associated with diabetes, cancer, heart disease, stroke, osteoporosis, and more.
American Heart Association
The AHA-endorsed diet, as one might guess from its promoter, is designed to be heart-healthy.2 “The American Heart Association’s Diet and Lifestyle Recommendations.” The American Heart Association. Updated:Apr 24,2014. (Accessed 27 April 2014.) http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyEating/The-American-Heart-Associations-Diet-and-Lifestyle-Recommendations_UCM_305855_Article.jsp It is built around relatively low-calorie foods that are theoretically rich in vitamins, minerals, and fiber and includes all major food groups for balanced nutrition. It is not a short term weight-loss diet, but is designed to be followed for the duration of one’s life. Specifically, it is centered around eating at least two 3.5-ounce servings of fatty ocean fish such as salmon, albacore tuna, mackerel, lake trout, or herring each week, which supplies you with omega-3 fatty acids that can lower your heart disease risk. It also includes eating at least three 1-ounce servings of fiber-rich whole-grain foods every day to theoretically help control your weight and cholesterol levels. And it also requires you to eat at least 4.5 cups of fruits and vegetables every day and four servings of nuts, legumes and seeds every week. It is the second most popular diet among physicians.
The biggest negative with this diet is its strong endorsement of grains–albeit unrefined grains. Yes, unrefined grains are better nutritionally than refined grains, and they certainly provide more necessary fiber. But whether whole or refined, many grains tend to trigger a strong glycemic response in the body, not to mention being highly allergenic. This eventually leads to insulin swings and depletion of the pancreas. Overall, other than a few exceptions which we’ll talk about later, I’m not a big fan of most grains–although when eaten in small amounts and in their unrefined form, they are not a problem for most people. But anything more than that is problematic. Sprouted grains are a much better choice and juices made from the grasses of the same grains–wheat, oat, barley–are even better. But these are not a part of the AHA diet.
Mediterranean
 As defined in the Medscape survey, the Mediterranean diet encourages followers to eat a variety of highly nutritious, plant-based foods, whole grains, fish, and poultry–with red meat consumed no more than once per month.
As defined in the Medscape survey, the Mediterranean diet encourages followers to eat a variety of highly nutritious, plant-based foods, whole grains, fish, and poultry–with red meat consumed no more than once per month.
The most important thing to note is that the base of this particular version of the Mediterranean diet is populated by grains. The diet’s foundation includes, bread, pasta, rice, couscous, polenta, other whole grains–and potatoes. This is not the version of the Mediterranean diet that I recommend (more on that later) and is a highly questionable choice.
Weight-loss, no calorie restriction and caloric restriction
As a combined category, this would probably move into third place among dietary choices for overweight physicians. Its primary appeal to physicians might very well be its non-specificity, which allows for a lot of leeway and flexibility of choice. Unfortunately, that also makes it very easy to fool yourself into thinking you’re on a diet when you’re not. But there’s an even bigger problem that we’ll discuss in a moment. First, however, it’s interesting that physicians would opt for caloric restriction as a way to lose weight considering that a 2006 study in the Archives of Internal Medicine found that one year of calorie restriction or exercise yielded similar weight loss, but only weight loss from calorie restriction produced significant decreases in bone-mineral density in older adults.3 Dennis T. Villareal, Luigi Fontana, Edward P. Weiss, et al. “Bone Mineral Density Response to Caloric Restriction–Induced Weight Loss or Exercise-Induced Weight Loss–A Randomized Controlled Trial.” Arch Intern Med. 2006;166(22):2502-2510. doi:10.1001/archinte.166.22.2502. http://archinte.jamanetwork.com/article.aspx?articleid=769549 Not really what you’re looking for as you age.
These are the kinds of programs that can allow you to lose weight as long as you follow them, but since they don’t involve permanent lifestyle changes, these are the kinds of programs that create yoyo weight-loss. You lose weight while religiously on the programs; then the weight begins to come back the moment you falter. In addition, since they don’t really regulate “what” you eat as much as how many calories you eat, they tend to allow for more glycemic swings or for the heavy consumption of conventional and processed meats, both of which are problematic.
Meals on-the-the-go
As discussed above, many physicians like to eat out at what are referred to as mid-level restaurants. This is as opposed to high-end dining and fast food. The majority of the mid-level restaurants favored by the physicians are local establishments–think a neighborhood Italian or Thai restaurant–with about half as many opting for mid-level chains–think Olive Branch and TGI Fridays. For the most part, this can be thought of as eating the typical American diet outside of the house.
Paleo
 I have discussed the Paleo diet in some detail previously. Although I find the theory behind it somewhat dubious, I nevertheless think that it has much to recommend it–but more for what it eliminates from your diet rather than for what it recommends you include in it. Eliminating all high glycemic starches and grains and dairy is not a bad place to begin any diet and has my vote. Replacing it with extremely high levels of meat is more open to debate. Specifically, the Paleo diet is based on eating whole foods from the food groups that hunter-gatherers theoretically would have thrived on during the Paleolithic era. These include fresh, lean meats such as grass-fed or free-range beef, pork, lamb, and poultry; fish and seafood; fresh fruits and vegetables; seeds and nuts; and healthful oils (olive, coconut, avocado, macadamia, walnut, and flaxseed). On the other hand, dairy products, cereals, legumes, refined sugars, and processed foods are excluded. According to the Medscape survey, approximately 6% of overweight physicians and 8% of normal- or underweight physicians follow a version of the Paleo diet.
I have discussed the Paleo diet in some detail previously. Although I find the theory behind it somewhat dubious, I nevertheless think that it has much to recommend it–but more for what it eliminates from your diet rather than for what it recommends you include in it. Eliminating all high glycemic starches and grains and dairy is not a bad place to begin any diet and has my vote. Replacing it with extremely high levels of meat is more open to debate. Specifically, the Paleo diet is based on eating whole foods from the food groups that hunter-gatherers theoretically would have thrived on during the Paleolithic era. These include fresh, lean meats such as grass-fed or free-range beef, pork, lamb, and poultry; fish and seafood; fresh fruits and vegetables; seeds and nuts; and healthful oils (olive, coconut, avocado, macadamia, walnut, and flaxseed). On the other hand, dairy products, cereals, legumes, refined sugars, and processed foods are excluded. According to the Medscape survey, approximately 6% of overweight physicians and 8% of normal- or underweight physicians follow a version of the Paleo diet.
As mentioned, I have a problem with the fundamental premise of the Paleo diet. The facts on the ground do not support it. There is a great deal of evidence that many Paleolithic peoples did in fact eat grains. And if eating meat were a prerequisite for health, then vegetarians as a group would have to be unhealthier than heavy meat eaters, and that just isn’t true. Study after study has shown that vegetarians (on a good vegetarian diet) tend to be healthier. I also have a problem with the consumption of high levels of meat–not because it causes heart disease, because in fact, the evidence strongly indicates that it does not. My issue is that there are multiple concerns associated with eating high levels of meat–just not heart disease.
For example, all meats, fish, poultry, and eggs are acid forming in the body. When metabolized, the proteins produce sulfuric acid and phosphoric acid in the body. And fats produce acetic acid. The way the body handles them is to neutralize them by converting them into acid salts; and it does this by combining them with the minerals sodium, potassium, magnesium…and most notably calcium, which it draws from the calcium bank in your body–your bones. At small amounts, this is not a problem. But as the consumption of meat increases, the end result could be a much higher incidence of osteoporosis down the road. On the other hand, higher levels of protein in the diet have been shown to be protective of bone health. The Paleo diet has not been in widespread use long enough to determine which way this plays out, but it is a concern. Also, eating high levels of meat disrupts intestinal flora resulting in a huge die-off of beneficial bacteria and an exponential increase in E. coli. And finally, epidemiological studies done at Harvard Medical School show that, “Men who eat red meat as a main dish five or more times a week have four times the risk of colon cancer than men who eat red meat less than once a month.”4 “Red meat and colon cancer.” The Harvard Medical School Family Health Guide. March 2008.(Accessed 30 April 2014.) http://www.health.harvard.edu/fhg/updates/Red-meat-and-colon-cancer.shtml They are also more than twice as likely to get prostate cancer.5 Esther M. John,Mariana C. Stern, Rashmi Sinha, and Jocelyn Koo1. “Meat consumption, Cooking Practices, Meat Mutagens and Risk of Prostate Cancer.” Nutr Cancer. 2011; 63(4): 525–537. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3516139/ And a recent study found that women who had more than one-and-a-half servings of red meat a day doubled their risk of hormone receptor–positive breast cancer.6 Cho, E., W.Y. Chen, D.J. Hunter, et al. “Red Meat Intake and Risk of Breast Cancer among Premenopausal Women.” Arch Intern Med166 (2006): 2253–2259. www.ncbi.nlm.nih.gov/pubmed/17101944
One of the arguments that Paleos use to counter this is that it’s not the meat, it’s the hormones and imbalance of fatty acids in commercial, grain fed meat VS grass fed beef. And yes, grass fed is far healthier than commercial grain fed. But unfortunately, science doesn’t support the fundamental premise of the argument. It’s pretty clear now that a key culprit is the PhIP amine generated from cooking meat at high temperatures.7 Deliang Tang, Jason J. Liu, Andrew Rundle, et al. “Grilled Meat Consumption and PhIP-DNA Adducts in Prostate Carcinogenesis.” Cancer Epidemiol Biomarkers Prev. Apr 2007; 16(4): 803–808. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2132437/ And that has nothing to do with hormones and grass fed VS grain fed.
Lacto-ovo vegetarian
The lacto-ovo vegetarian diet is the most common vegetarian diet. It excludes all animal “flesh,” including seafood. But it allows for the consumption of all dairy products and eggs.
On the downside, it also includes large amounts of fruits and fruit sugars, not to mention a large amount of grains, legumes, and quite often soy.
Gluten free
About 2 million Americans have celiac disease, a genetic inability to process key proteins–gluten and gliadin–in the small intestine. Instead of being digested in predisposed people, these proteins trigger an autoimmune response that results in inflammation of intestinal tissue, pain, chronic constipation and/or diarrhea, anemia, and fatigue. It is now being diagnosed in asymptomatic people as a result of more sensitive antibody screening. Not surprisingly, the one dictum of the gluten free diet is eliminating all sources of gluten. That means no wheat, barley, or rye–or anything made with them. It also means, unless they are specially formulated to be gluten free, no pastas, breads, baked goods, crackers, cereal, granola, beer, or sauces.
On the negative side, it does allow for a wealth of high glycemic foods such as potatoes and rice, not to mention the fact that many of the non-gluten baked goods now offered tend to be high in sugar.
Vegan
You would think the vegan diet is similar to the lacto-ovo diet–just without the dairy and eggs. However, avoiding all animal proteins tends to necessitate some major adjustments to get enough protein. Yes, you can mix your vegetables and grains to get a mix of amino acids that provide your basic protein needs, but if you need anything beyond the basic levels of protein on this diet–if you pursue athletic endeavors or are recovering from surgery or illness, for example, or are over 55–then you have to notably increase your consumption of nuts, seeds, legumes, and grains…or worst of all high levels of soy to get enough protein. And again, like all of the diets discussed so far, except for the Paleo diet, the base of the vegan food pyramid is grains.
Ornish
 The Ornish diet focuses on fat–virtually eliminating almost all fats even supposedly beneficial ones–from the diet.8 http://www.ornishspectrum.com/proven-program/nutrition/ For similar reasons, it limits consumption of red meat to small portions no more than once monthly, and of lean poultry to no more than once daily (if that), but it allows up to 2 servings daily of egg whites and fish. Ideally, the diet comprises 10% fat, 20% protein, and 70% carbohydrates. It is backed by 35 years of scientific research (virtually all of which has been conducted by Dr. Ornish) that has shown that the program works for losing weight; lowering cholesterol and blood pressure; helping to prevent or treat diabetes, heart disease, cancer, and other conditions; and that it helps improve psychological well-being as well.
The Ornish diet focuses on fat–virtually eliminating almost all fats even supposedly beneficial ones–from the diet.8 http://www.ornishspectrum.com/proven-program/nutrition/ For similar reasons, it limits consumption of red meat to small portions no more than once monthly, and of lean poultry to no more than once daily (if that), but it allows up to 2 servings daily of egg whites and fish. Ideally, the diet comprises 10% fat, 20% protein, and 70% carbohydrates. It is backed by 35 years of scientific research (virtually all of which has been conducted by Dr. Ornish) that has shown that the program works for losing weight; lowering cholesterol and blood pressure; helping to prevent or treat diabetes, heart disease, cancer, and other conditions; and that it helps improve psychological well-being as well.
Its biggest problems from my perspective are, first, that it eliminates too many fats. Despite Dr. Ornish’s research, the right kind of fats in moderate amounts play a key role in health. Too little fat in the diet, at the most basic level, can result in energy loss and deficiencies in the fat soluble vitamins which are stored in the liver and fatty tissue–specifically, vitamins A, D, E, and K. In addition, there are other more specific fat based nutrients that are also essential for health and are likely to be deficient in the Ornish diet. These include things like GLA, DGLA, and CLA to name just three. The diet’s second major problem, once again, is that the base of its food pyramid is unrefined whole grains…in abundance. It also recommends lots of soy, with the lone exception of soy protein powders.
Conclusion

So what did we learn from all of this? Well, unlike end-of-life choices where it’s a “Do as I say, not as I do” approach for doctors, when it comes to diets, it would appear that they simply don’t know what to say…because they don’t know themselves. As we can see, doctors’ choices when it comes to diet are all over the map. Despite the fact that there are “officially” endorsed diets like the AHA diet, which a number of doctors do indeed claim to follow, the majority of doctors follow no diet at all, living on burgers and fries and food on-the-go. To put it simply, they’re as confused as the rest of us.
The bottom line is why would you ask advice from people who are that confused? And keep in mind, doctors don’t study diet and nutrition in medical school–at least not to any notable degree. Most of what they think they know comes from reading an article in a medical journal or reading about the results of some epidemiological study that may or may not be fatally flawed. If you read two good books on nutrition, you know more than 90% of the doctors dispensing nutritional advice. That wouldn’t necessarily be a major problem if it weren’t for the fact that these same doctors don the mantle of expertise and tell you what diet to follow…based on their own ignorance. It is the height of arrogance. Look, it makes all the sense in the world to ask your doctor’s advice when it comes to most diseases and trauma. They study that. But it makes no sense to ask most doctors about diet and nutrition. They’re really pretty ignorant about it–sorry to put it so bluntly.
So what diet do I recommend?
After intensively studying this field for 48 years now, my diet of choice is the Mediterranean diet–but a very particular form of it. Historically speaking, the Mediterranean diet is not “actually” the diet of any country or area; instead, it is “inspired” by the traditional dietary patterns of the peoples of southern Italy, Greece, and Spain. The more generic forms of the diet–and the form followed by most of the physicians in the survey–center around high consumption of olive oil, legumes, unrefined cereals, fruits, and vegetables, with moderate to high consumption of fish, moderate consumption of dairy products (mostly as cheese and yogurt), moderate wine consumption, and low consumption of meat and meat products.
The version of the Mediterranean diet that I recommend modifies that as follows:
- High consumption of non-starchy vegetables and greens. Although the Mediterranean diet is not necessarily a vegetarian diet, fresh vegetables and salad greens are its single most important component. Fresh vegetables have high nutrient density. That is: they provide high levels of nutrition with the fewest number of calories. Broccoli, for example, provides more protein per calorie than a lean steak. Note: that’s per calorie, not per ounce or pound; and it’s not a complete protein. You need other amino acid rich foods to complement it so that you can maximize its protein value. But that said, fresh vegetables are among the most nutrient dense foods available. Vegetable juices are also extremely healthy. Just don’t go crazy with the high sugar vegetables such as beets and carrots.
- Moderate to high consumption of wild caught fish (if desired…and if it’s still available).
- Moderate consumption of organic, free-range chicken or turkey (if desired). Remember: non-organic poultry is likely to contain high levels of arsenic and chicken tumors.
- Moderate consumption of nuts and seeds (if not allergic). And keep in mind that sprouting nuts and seeds–if you can find any that are not pasteurized nowadays–dramatically improves their nutrition level and health benefits, while reducing the possibility of any adverse reactions. Among the best nuts to eat are almonds and walnuts, and for seeds we’re looking at sunflower, flax, and chia seeds.
- Moderate consumption of chlorella, spirulina, and blue green algae (if not allergic). They are a great source of protein (albeit quite expensive). They are also nutrient dense and are great for removing toxins and heavy metals from the body, especially chlorella.
- Moderate consumption of fruit. Fruits are incredibly high in antioxidants, which is good. But they are also very high in sugars, which is not so good. Eating whole fruit helps modify the sugar hit. If you drink fruit juices, then you absolutely must restrict yourself to fresh squeezed–and dilute them with fresh water when you drink them…to cut the sugar hit.
- Moderate consumption of oils and fats such as:
- Olive oil.
- Walnut oil.
- Avocado oil.
- Coconut oil.
- Organic butter from grass fed cows.
- With supplemental krill oil, squid oil, fish oil, and flax lignans.
- Avoid like the plague all manmade trans fats (natural ones are fine) and all ultra-refined, high omega-6 vegetable oils (the kind that can last on your shelf for years without ever going rancid).
- Moderate consumption of organic, certified-humane eggs (if desired).
- Low to moderate consumption of organic, free-range meat and meat products (if desired).
- Low consumption of organic, raw dairy products–mostly as yogurt and cheese (if desired). Whey is certainly a concentrated source of supplemental protein, but it’s also extremely high in allergens. I would keep consumption moderate to low.
- Low consumption of legumes and, if you eat them, make sure you soak them before cooking and then cook them well before eating.
- Low consumption of unfermented soy products such as tofu and soy milk. Adults can consume moderate levels of fermented soy, but children should avoid all soy as the phytoestrogen content is just too much for them.
- Low consumption of unrefined, organic grain products. (Avoid the newer strains of non-organic high gliadin wheat.) And if you have celiac disease, then avoid them altogether. Do not substitute with high glycemic, non-gluten knock offs. Since this diet recommends low consumption of these foods anyway, simply eliminating them is not that big a sacrifice. If you don’t have a gluten problem, barley is not a bad choice as it is low glycemic. Even better is pre-sprouted barley, which is a nutritional powerhouse.
- Extremely low (or no) consumption of high glycemic refined grains, starches (e.g. potatoes), isolated sugars, and any modern, high-gliadin, genetically engineered strains of wheat.
It is said that we dig our graves one forkful at a time. There is much truth in that statement. Likewise, making smart dietary choices gives you much better odds of living a long, healthy life. Not a guarantee–just better odds. In the end, it’s your body, your life, your choice. Only you can determine what that choice will be–not your doctor.

References
| ↑1 | Carol Peckham. “Medscape Physician Lifestyle Report 2014.” January 23, 2014. Medscape. http://www.medscape.com/features/slideshow/lifestyle/2014/public/overview#1 |
|---|---|
| ↑2 | “The American Heart Association’s Diet and Lifestyle Recommendations.” The American Heart Association. Updated:Apr 24,2014. (Accessed 27 April 2014.) http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyEating/The-American-Heart-Associations-Diet-and-Lifestyle-Recommendations_UCM_305855_Article.jsp |
| ↑3 | Dennis T. Villareal, Luigi Fontana, Edward P. Weiss, et al. “Bone Mineral Density Response to Caloric Restriction–Induced Weight Loss or Exercise-Induced Weight Loss–A Randomized Controlled Trial.” Arch Intern Med. 2006;166(22):2502-2510. doi:10.1001/archinte.166.22.2502. http://archinte.jamanetwork.com/article.aspx?articleid=769549 |
| ↑4 | “Red meat and colon cancer.” The Harvard Medical School Family Health Guide. March 2008.(Accessed 30 April 2014.) http://www.health.harvard.edu/fhg/updates/Red-meat-and-colon-cancer.shtml |
| ↑5 | Esther M. John,Mariana C. Stern, Rashmi Sinha, and Jocelyn Koo1. “Meat consumption, Cooking Practices, Meat Mutagens and Risk of Prostate Cancer.” Nutr Cancer. 2011; 63(4): 525–537. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3516139/ |
| ↑6 | Cho, E., W.Y. Chen, D.J. Hunter, et al. “Red Meat Intake and Risk of Breast Cancer among Premenopausal Women.” Arch Intern Med166 (2006): 2253–2259. www.ncbi.nlm.nih.gov/pubmed/17101944 |
| ↑7 | Deliang Tang, Jason J. Liu, Andrew Rundle, et al. “Grilled Meat Consumption and PhIP-DNA Adducts in Prostate Carcinogenesis.” Cancer Epidemiol Biomarkers Prev. Apr 2007; 16(4): 803–808. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2132437/ |
| ↑8 | http://www.ornishspectrum.com/proven-program/nutrition/ |












The main cautionary regarding
The main cautionary regarding following a medical doctors dietary advice is a first step (and this article certainly displays why). Further steps need to be taken for an individual to be more fully informed regarding their best dietary choices.
Interesting to hear that there are versions of the “Mediterranean Diet”. It seems (with a few exceptions) that Jon’s version could possibly be likened to the dietary fundamentals presented in “Nourishing Traditions” (which he makes no mention of at all in this article). One exception is the recommended “Low consumption of unfermented soy products such as tofu and soy milk”. More information is needed to substantiate a few more of his recommendations such as the notion that “Whey is … extremely high in allergens”. That idea deserves a complete article fully discussing this as well as the recommended “Low consumption of organic, raw dairy products”.
I suppose that my weekly consumption of four gallons of raw goat milk clabber would not be considered “low consumption” and yet I have never felt more well-nourished and physically comfortable than ever before!
Diet is firstly an individual matter. There is no universal diet. The idea of such is not supported by traditional wisdom. I’m glad that Jon’s diet works for him however it can not be expected to work for everyone. It is not a diet I would necessarily recommend.
The most well-documented dietary findings for a wide variety of truly healthy peoples remains to be “Nutrition and Physical Degeneration” by Weston A. Price. Why is that book not referenced here?
Jon mentions that Evan grass
Jon mentions that even grass fed beef is not good for you at high temperatures, so I never cook mine at high temps. A steak cooked in butter or ghee on low is devine!
I found this article
I found this article interesting as I have followed all these diets with the exception of vegan and ornish. Those both seemed too extreme to me. I think that many people have a hard time succeeding on these various diets because to feel really well and/or to lose/gain appropriate weight requires a level of awareness of one’s own symptoms and continued research of those symptoms to find the right individual diet. I certainly feel that way about my journey with diets and my many failures.
I was able to lose weight following a paleo plan but ultimately found that my body could not tolerate the histamine hit of so much meat in which the histamines are much higher when slow cooked or left over (cooking for the week) Now I follow more of the modified mediterranean diet he recommends with very little grain. I also added raw potato starch as a resistant starch component which has helped with sleep and ibs. I continue to search for the diet that I feel best eating and that is low to moderate in toxicity to my body.
Luckily there are many more opportunities today to be your own best advocate for health. You can do much without conventional doctors. Even ordering tests which can help you decipher your individual issues such as gut health or testing for genetic mutations. This can allow you to slowly refine your diet to one that is as nutritionally dense, and of low toxicity to your own body.
I’d like to see a diet menu.
I’d like to see a diet menu. Sometimes it helps to see one so I can make a menu for my family since I am not a very good cook. Breakfast is the most difficult for my kids since they like oatmeal everyday and dislike eggs. Any link would be very welcome.
THANKS!
I know I am an exception but
I know I am an exception but at 74 and low body fat I need more calories when I work on my retirement farm 3 days a week. I find Potatoes that I raise myself to be the best choice on those days.
I microwave them and mash them with coconut oil, mined sea salt and spices. I work on that meal until my body signals that I need more calories.
On alternate days when I am doing therapy work I eat a more nutrient dense diet
The courageous men and women
The courageous men and women who put in over 15 years in medical school and internships should never be doubted. I owe my life to my doctors. I had a heart attack excercising at a gym when I was 46. I was clinically dead. I was told it took 15 minutes to revive me. I had a 90% blockage in one of my arteries and an 80% blockage in my aorta. I had to have two stents via catheters. My cardiologist prescribed me Lipitor of which I take everyday along with Plavix as a blood thinner, Dyazide for water retention and Amplodopine for my BP. Today I’m 56 years old with normal cholesterol (thank you Lipitor) and a safe BP reading. I became a vegaterian a decade ago as advised by my hosptial’s nutritionist as the safest option for my cardiovascular health. I also jog at least one mile a day and I’m thankful everyday to be alive and healthy.
Of course MDs do not know
Of course MDs do not know about diet. They even once believed smoking wasn’t bad for people; some even stood up for the practice. My sister’s new young MD when asked (because I bug her all the time about it) if it was important to take ‘magnesium’, responded, “We don’t know much about that, it would be best to ask your pharmacist”. Now that is telling.
MDs know about illnesses, or piano falls on head, etc., but when it comes to health, they know little; there is no money in it. And their only resources are chemical prescriptions and surgery.
It’s the same with vets. Look at all the kibble they well in their establishments. My little dog got terrible liver cancer age 14. I fed her the best prescribed dog food in a bag possible. My Corgi, now sixteen and one month is losing her hind quarters, part of the problem with breeds, but otherwise she is healthy, hungry and happy. I expect she will live another year.
My mum died in hospital because the establishment would not allow her to bring in her one supplement, Magnesium. Three days later her electrolytes went out of balance and she died. It’s been 21 years now and I still have not forgiven the system.
Been taking Borax nearly 9 years and a recent Dentist was amazed at my ‘Extremely strong bones”; for any age when I asked if he meant for my age, 64 at the time. No doctor or dentist knows how valuable the simple mineral Borax/boron is to our health. Pneumonia can be defeated with this simple mineral.
Best to do your own study, far and wide; and it helps if you have a naturopath to visit.
Namaste and care,
mhikl
That is telling! Thank you
That is telling! Thank you for sharing.
I am curious to know more
I am curious to know more about the recommendation against legumes given that in the case of all Blue Zone populations, legumes are an important part of their diet. (Blue Zones are regions that have been found to have extremely long-lived, healthy populations.)