We’ve all heard the expression, “You can’t see the forest for the trees.” Its meaning is simple: if you look too closely at small details, you miss the big picture. And so it is when it comes to studies that explore the relationship between gum disease and various illnesses. When each study is viewed as a single tree, no one sees the forest.
What specifically am I talking about? What is the trigger for today’s newsletter?
It’s a new study just published in the Journal of Periodontology that once again confirms the connection between gum disease and arthritis. But that’s just the tip of iceberg (to use another idiomatic cliché). To understand what I’m talking about, it’s important to look at the whole enchilada (sorry, I’m on a roll). And with that in mind, let’s explore the entire forest as it relates to gum disease and the whole spectrum of chronic illnesses. And even more importantly, we’ll examine how that ties into the principles of the Baseline of Health® program.
Gum disease and rheumatoid arthritis
Let’s begin by looking at the study from the Journal of Periodontology that I just cited above. In summary, the study concluded that non-surgical periodontal therapy had a beneficial effect on the signs and symptoms of rheumatoid arthritis (RA), regardless of the medications used to treat the condition. On the other hand, anti-TNF-α therapy (a frequently used treatment for arthritis) without periodontal treatment had no significant effect on the periodontal condition. Or as the BBC said, commenting on the study, “People who have both gum disease and rheumatoid arthritis can relieve both conditions by treating their mouth infection.”
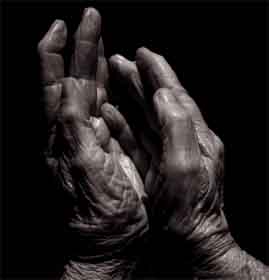 But this isn’t the first time the connection between periodontitis and RA has been noted. For example, back in 2005, another study published in the Journal of Periodontology found that periodontitis and rheumatoid arthritis (RA) appear to share many pathologic features. This study reviewed the common mechanisms of these two common chronic conditions and found that emerging evidence suggested a strong relationship between the extent and severity of periodontal disease and RA.
But this isn’t the first time the connection between periodontitis and RA has been noted. For example, back in 2005, another study published in the Journal of Periodontology found that periodontitis and rheumatoid arthritis (RA) appear to share many pathologic features. This study reviewed the common mechanisms of these two common chronic conditions and found that emerging evidence suggested a strong relationship between the extent and severity of periodontal disease and RA.
While the study was unwilling to declare the relationship causal, it did state that it was clear that individuals with advanced RA were more likely to experience more significant periodontal problems compared to their non-RA counterparts, and vice versa. In the end, it made a case that these two diseases could be very closely related through a common underlying dysfunction of fundamental inflammatory mechanisms. Although the study’s authors stated that the nature of such dysfunction was unknown, they nevertheless declared that accruing evidence supported the notion that both conditions manifested as a result of an imbalance between pro-inflammatory and anti-inflammatory cytokines. The clinical implication, as far as the study was concerned, was that patients with RA should be carefully screened for their periodontal status.
Well, that seems pretty straight forward. Arthritis and periodontal disease seem to be connected. Where’s the confusion? What do forests and trees have to do with it? To answer that question we need to take a step back and look at more than just the single tree of rheumatoid arthritis.
Gum disease and respiratory illness
The association between poor oral health and chronic lung disease has been known for close to a decade. What’s the connection? As it turns out, inhaling bacteria from the mouth and throat can lead to pneumonia. Additionally, dental plaque buildup creates a dangerous source of bacteria that can also be inhaled into the lungs. Specifically, studies have found that lung function appears to diminish progressively as periodontal attachment loss (a measure of the severity of the disease) increases.
Additionally, other studies have confirmed that higher dental plaque scores confer a greater risk of contracting ventilator-associated pneumonia for patients in acute care facilities, particularly for patients with a greater severity of illness.
The connection between gum disease and lung disease, thus appears, strong. So where do we stand? We’ve now explored the relationship between gum disease and rheumatoid arthritis and respiratory illness. Anything else?
Gum disease and diabetes
As with respiratory disease and arthritis, the connection between diabetes and gum disease has been known for some time. Specifically, it has been demonstrated that people with diabetes are more likely to have periodontal disease than people without diabetes. One reason is probably because diabetics are more susceptible to contracting infections. Uncontrolled diabetes impairs neutrophils (a particular kind of white blood cell), which are a primary defense against bacterial infection. Thus, because periodontal disease is a bacterial infection, people with uncontrolled diabetes are more likely to have it since their immune systems are less able to defend against it, and their conditions are likely to be more severe. In fact, periodontal disease is often considered one of the primary complications of diabetes. It should also be noted that those people who are unable to control their diabetes are at particular risk.
Another possible risk factor is that diabetes thickens blood vessels, which in itself may lead to an increased risk of gum disease. Blood vessels deliver oxygen and nourishment to body tissues, including the mouth, and carry away the tissues’ waste products. Since diabetes causes blood vessels to thicken, this slows the flow of nutrients and the removal of harmful wastes from the gums which can weaken the resistance of gum and bone tissue to infection.
But that’s not all. Research has emerged that suggests that the relationship between periodontal disease and diabetes goes both ways — periodontal disease may make it more difficult for people who have diabetes to control their blood sugar. That’s right! Severe periodontal disease can increase blood sugar (not to mention triglyceride levels), contributing to increased periods of time when the body functions with high blood sugar. Why? Because any type of infection can cause blood-sugar levels to rise. This increases the need for insulin. Conversely, if you treat the periodontal infection successfully, the need for insulin may decrease, thus making the diabetes easier to control.
So now we’ve gone from arthritis to respiratory illness to diabetes. Are there any other trees we need to look at relative to gum disease?
Gum disease and Alzheimer’s
A 2005 study of dementia in identical twins found that exposure to inflammation early in life, such as experienced in gum disease, quadruples one’s risk of developing Alzheimer’s disease. In fact, the connection between inflammation and Alzheimer’s has been well established. It has been proposed, in fact, that inflammation could be the actual start of a chain reaction that leads ultimately to Alzheimer’s disease. Normal brain molecules are disrupted as a result of inflammation and this can cause amyloid beta proteins in the brain to misfold. Misfolded amyloid beta proteins are thought to have a critical role in the development of Alzheimer’s. According to Jeffery W. Kelly, one of the researchers associated with the study, the inflammation process might occur years before the onset of Alzheimer’s and be the result of any number of infections people can contract — again, including gum disease.
Gum disease and heart disease
And then there’s the connection between gum disease and heart disease. The problem is that periodontal bacteria can enter the bloodstream and travel to major organs and begin new infections. Research has suggested that this may contribute to the development of heart disease, the world’s leading cause of death. Several studies appearing in the Journal of Periodontology examined this connection:
- In one study, researchers looked at 150 individuals with periodontal diseases and found that the total number of periodontal bacteria in plaque below the gum-line was higher in individuals that had suffered from an acute heart attack.
- The second study found that the same DNA from different kinds of periodontal bacteria in plaque was also in the patients’ heart arteries.
- The third and most recent study investigated how the severity of periodontal disease and the number of remaining teeth relates to heart attacks and hypertension. Results of this study examining 4,254 subjects offered a clear link between dental health and heart disease. The number of diseased periodontal pockets was significantly related to hypertension, no matter the age of the subject. Even more alarming for middle-aged people is the finding that the number of teeth was inversely associated with heart attacks. The fewer the teeth, the more likely a heart attack.
The forest surrounding periodontal disease
 So what does it all mean? It means that if you take each study in isolation, you miss the forest. The forest is that the true significance of gum disease is not that it is associated with any one disease in particular, but rather, that it is associated with many diseases simultaneously…and with a general degradation of health. In fact, periodontal disease can be linked not only to arthritis, lung disease, diabetes, Alzheimer’s, and heart disease as discussed above, but also to stroke, stomach ulcers, obesity, renal disease, obesity, pancreatic cancer, and even an increased risk of having a preterm, low birth weight baby.
So what does it all mean? It means that if you take each study in isolation, you miss the forest. The forest is that the true significance of gum disease is not that it is associated with any one disease in particular, but rather, that it is associated with many diseases simultaneously…and with a general degradation of health. In fact, periodontal disease can be linked not only to arthritis, lung disease, diabetes, Alzheimer’s, and heart disease as discussed above, but also to stroke, stomach ulcers, obesity, renal disease, obesity, pancreatic cancer, and even an increased risk of having a preterm, low birth weight baby.
The bottom line is that good oral health is not just about your smile, it’s about your life. And how big is the problem? Several years ago, the Surgeon General of the United States, David Satcher, called oral disease the “silent epidemic” because so many people have it without even realizing it. It is a silent epidemic because the symptoms are so innocuous in the beginning that it is far too easy for people to ignore them. It is estimated that more than 75% of American adults have some form of gum disease, but according to a major survey, only 60% are aware they even have a problem. And it’s not just the United States. The statistics are similar throughout the world. In Singapore, for example, it is estimated that 80% of the population has some level of gum disease.
What to do about gum disease
Beyond the obvious things your dentist tells you, I’d like to talk about four things in particular that you are less likely to know about: avocado soy unsaponifiables, proteolytic enzymes, green tea, and garlic based formulas.
1. Avocado soy unsaponifiables (ASU)
It is now understood that one biochemical in particular is responsible for the erosion of oral structures — literally eating away at your jawbone and the ligaments that hold your teeth to your jaw. This oral toxin is called Interleukin-1beta (IL-1beta), and it has been referred to as the “common mediator of the inflammation process.” Your body’s counter measure to IL-1beta is a family of biochemicals called “Transforming growth factor-beta.” TGF-beta has been identified as one of the factors capable of counteracting IL-1beta’s destructive effects and plays a key role in tissue regeneration. Unfortunately, one of the effects of IL-1beta is that it inhibits the production of TGF-beta, the very substance that can counteract it and repair the damage. Luckily we have ASU.
A French study found that ASU can exert a preventive action on the erosive effects exerted by IL-1beta in periodontal diseases. Specifically, researchers found that ASU stimulated the production of the protective TGF-beta family of growth factors. In other words, ASU helped the periodontal ligament and oral bone cells protect themselves by inhibiting the erosive effect of IL-1beta. According to the researchers, these “findings support the hypothesis that ASU could exert a preventive action on the deleterious effects exerted by IL-1beta in periodontal diseases.”
A second French study found that ASU might be beneficial in patients with gingival inflammation and periodontitis by preventing the erosive effects of IL-1beta that occur in periodontal diseases.
And finally, a third French Study showed that avocado and soybean unsaponifiables protect all types of gingival elastic fibers from degradation by HLE. HLE is one of several hydrolytic (water removing) enzymes contained in neutrophils. Physiologically, it digests foreign material ingested by immune cells. However, when triggered by the inflammation and infection associated with gingivitis, it attacks the elastic and preelastic fibers that help hold your teeth in place. This destruction is a hallmark of periodontal disease. Thus the study concluded that ASU may be beneficial in patients with gingival inflammation and periodontitis since HLE plays a major role in these disease states.
For more information on ASU based formulas, check out: Chronic Joint Pain and Inflammation.
2. Proteolytic enzymes
Saliva plays a major role in the health of the oral cavity and the entire body. Saliva is made up primarily of water but also contains digestive enzymes such as amylase and minerals. In addition, certain supplemental proteolytic enzymes such as seaprose-s, nattokinase, and serrapeptase seem to have the ability to make their way from your blood into your saliva, where they can dissolve dental plaque and wash away the bacteria that cause dental caries. Here at the Foundation, we have received a number of emails from people using formulas based on these enzymes indicating that they may indeed help. For example:
- “I’ve always had challenges with my dental health. Since taking the proteolytic enzymes, I’ve noticed there is no build up of plaque on my teeth!”
- “She then told me that she had had a long time problem with plaque on her teeth. Well, she said that morning she noticed that all of the plaque was gone! This was after being on the [enzymes] only 5 days. Neither of us expected that!”
For more information on proteolytic enzyme based formulas, check out: A Patent Pending Proteolytic Enzyme Formula.
3. Green tea
The old alternative health standby, green tea, has been shown to be effective in controlling periodontal disease. In studies at the Kyushu University Faculty of Dental Science, Fukuoka, Japan, a modest inverse association between the intake of green tea and periodontal disease was demonstrated as was a reduction in gum bleeding on probing. The more people drank, the greater the benefit.
4. Garlic based formulas
Garlic based formulas have a long and proven history in counteracting periodontal disease. Periodontitis is often treated with common antibiotics such as amoxicillin, but antibiotic resistance is a growing problem. As I’ve discussed in previous newsletters, garlic based formulas avoid this resistance problem. It should be noted that a garlic extract equivalent to three garlic bulbs was proven highly effective against many oral pathogens. It should also be noted that my Super ViraGon® formula contains the equivalent of 30 cloves of fresh garlic — 10 times as much.
Conclusion
Once again, we are forced to accept the value of the Baseline of Health® approach in dealing with virtually all chronic health conditions since so many conditions are related and mutually reinforcing. The premise is simple. Don’t look for magic bullets. Do everything, and do it all at once. If you were to deal with heart disease, for example, by taking standard heart medications, you would miss the role gum disease plays in your condition. Likewise diabetes, lung disease, and Alzheimer’s. Treat the disease in isolation by limiting yourself to pharmaceutical drugs to control symptoms, and you significantly reduce your chances of obtaining a positive outcome since so many factors are outside of that particular drug’s purview.
On the other hand, if you were to treat your gum disease by merely following the standard dental protocols, you would also miss out — for example, by not dealing with the role that diabetes might play in your periodontal condition.
In the end, most chronic illness, whether it be cancer, diabetes, arthritis, or Alzheimer’s — take your pick — has more than a single cause and has ramifications that extend far beyond its immediate symptoms. Cancer and your immune system, for example, have a symbiotic relationship, as does diabetes and virtually all of the major systems of your body — not to forget, Alzheimer’s and the protein degradation that happens over time in every single organ in your body. It is these echo effects that so undermine the efficacy of magic bullets, and scream out for the holistic approach of the Baseline of Health®.

Something to chew over the next time you consider treatment for periodontal disease…or for any chronic illness.